
A new histopathological location of parathyroid gland with high possibility of unintended parathyroidectomy
Highlight box
Key findings
• New histopathological location of parathyroid gland.
What is known and what is new?
• Unintended removal of intrathyroidal parathyroid gland is inevitable during thyroidectomy.
• Partially buried parathyroid gland, which is not intraoperatively visible to the naked eye, has been newly discovered.
What is the implication, and what should change now?
• Partially buried parathyroid gland can act as a risk factor for unintended parathyroidectomy comparable to intrathyroidal parathyroid gland during thyroid surgery.
• It is worth using newly developed visualizing techniques to preserve partially buried parathyroid glands.
Introduction
The widely performed surgical technique of thyroidectomy has been capsular dissection, and the goal is to reduce intraoperative injury of parathyroid gland or unintended parathyroidectomy through meticulous capsular dissection. Nevertheless, surgeons are occasionally embarrassed by a pathologic report indicating parathyroid glands along with the thyroid specimen, and the proportion of unintended parathyroidectomy has been known to be ranged from 5.2% to 21.6% (1,2). The histopathological locations of unintentionally removed parathyroid glands have been reported to be intrathyroidal, subcapsular, and extracapsular (3-7). Traditionally, the extracapsular parathyroid gland has been defined as lying outside the capsule of thyroid gland while the intrathyroidal parathyroid gland as being completely surrounded by the parenchyme of thyroid gland (8). The subcapsular parathyroid gland has been defined as lying just beneath the capsule but completely outside the thyroid parenchyma. Ideally, capsular dissection seems to preserve the subcapsular parathyroid glands during the operation, but, in practice, unintended removal of parathyroid gland can be found even with meticulous capsular dissection. Therefore, this study was initiated due to the possibility of new histopathological location under the capsule but was difficult to detect with the naked eye as part of reducing unintended subcapsular parathyroidectomy.
This study aimed to investigate the new histopathological location of parathyroid gland with high possibility of unintended parathyroidectomy along with incidence of unintended parathyroidectomy during our thyroid operation. We present this article in accordance with the STROBE reporting checklist (available at https://gs.amegroups.com/article/view/10.21037/gs-23-282/rc).
Methods
Data from 761 consecutive patients who underwent any type of thyroidectomy procedure (hemithyroidectomy or total thyroidectomy with or without neck dissection) in Department of Otorhinolaryngology-Head and Neck Surgery at Korea University, Guro Hospital from January 1, 2013 to December 31, 2017, were collected for this study through a retrospective review of the charts.
All patients with benign or malignant thyroid disease admitted for thyroidectomy in this 5-year period were included. Patients who underwent thyroid operations for parathyroid disease diagnosed preoperatively or intraoperatively (n=11), those with repeated thyroid operations due to recurrent thyroid disease or residual malignant thyroid disease (n=14), those with parathyroid autotransplantation due to unintended excision or devascularization of a parathyroid gland during operation (n=27), and those who underwent extensive thyroid procedures, such as laryngectomy, tracheal resection or median sternotomy, due to locally advanced thyroid cancer (n=5) were excluded. Finally, the data of the remaining 704 cases were analyzed.
All thyroidectomy procedures were performed in a similar fashion by two surgeons (J.G.C. and J.S.W.) with over 10 years of experience in thyroid surgery. The procedures involved careful capsular dissection in attempts to identify and preserve the parathyroid glands with intact vascularity. Excessive and unnecessary dissections for locating missing parathyroid glands were avoided. Therapeutic unilateral or bilateral lateral neck dissections were performed for a clinical N1 stage in addition to bilateral central neck dissection. According to surgeons’ policy, prophylactic central neck dissection was not performed for a clinical N0 stage of patients who received total thyroidectomy alone.
Pathological reports and histological slides of all specimens were reviewed to verify the presence of the parathyroid glands with the number of glands removed and their histopathological location. To find the histopathological factors that make it difficult for surgeons to find parathyroid glands, their location in the specimen was classified as intracapsule and extracapsule based on the review of the slides by a pathologist. Intracapsular location was defined as the parathyroid glands located beneath the capsular propria of the thyroid gland and it traditionally included intrathyroidal and subcapsular location. Extracapsular location was defined as the glands outside the thyroid capsule. Under the assumption that there would be parathyroid gland partially buried in the parenchyme or partially visible through the capsule of thyroid glands, the intracapsular location of the parathyroid glands was further classified as completely buried in the thyroid parenchyme, partially buried, and subcapsular locations (Figure 1).

Depending on the histopathological location of unintentionally removed parathyroid glands, patients were divided into two groups: partially buried and subcapsular location, versus extracapsular location. The completely buried parathyroid gland was excluded from the comparison because sacrifice of parathyroid glands is inevitable even with capsular dissection. Extent of surgery, pathological diagnosis, and the presence of extrathyroidal extension were compared between two groups.
Statistical analysis
Statistical analysis of Chi-squared test was performed for categorical variables. Data are expressed as mean ± standard error of the mean, unless otherwise specified. All tests were two-sided and the level of statistical significance was established at P<0.05.
Ethical statement
This study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the Institutional Review Board of Korea University Guro Hospital (No. 2018GR0229) and individual consent for this retrospective analysis was waived.
Results
Among the 704 patients who underwent thyroidectomy, hemithyroidectomy was performed in 221 patients (31.4%) and total thyroidectomy with or without neck dissection in the others (n=483, 68.6%). Cancer was pathologically diagnosed in 515 patients (73.2%). The incidence of unintended parathyroidectomy was 12.8% (n=90). Among these cases, more than two parathyroid glands were removed in 11 patients (two glands in nine patients and three glands in two patients), who underwent total thyroidectomy with neck dissection; thus, 103 parathyroid glands were detected in 90 cases. The demographic and clinical data of the study group are presented in Table 1.
Table 1
| Variables | Values |
|---|---|
| Age (years), mean ± SE | 53±2.9 |
| Sex, n (%) | |
| Male | 98 (13.9) |
| Female | 606 (86.1) |
| Operation, n (%) | |
| Hemithyroidectomy | 221 (31.4) |
| Total thyroidectomy only | 372 (52.8) |
| Total thyroidectomy with neck dissection | 111 (15.8) |
| Histopathological features, n (%) | |
| Benign | 189 (26.8) |
| Malignant | 515 (73.2) |
| Incidental parathyroidectomy, n (%) | 90 (12.8) |
SE, standard error.
The histopathological locations of the unintentionally removed parathyroid glands were classified as intracapsular and extracapsular. The intracapsular was subclassified as completely buried, partially buried, and subcapsular (Figure 2). Among 103 unintentionally removed parathyroid glands, 74 glands (71.8%) were found intracapsular and 29 extracapsular (Table 2). Preservation was failed for the 74 parathyroid glands found at the intracapsular location. Among them, 57 parathyroid glands (55.4%) were found in difficult locations; 40.8% of the parathyroid glands (n=42) were completely buried in the thyroid parenchyme (Figure 2A), and 15 glands were partially buried, where it is usually difficult to locate the parathyroid glands (Figure 2B). The remaining 17 parathyroid glands (16.5%) in the intracapsular location were found above the parenchyme of thyroid gland (subcapsular location, Figure 2C). The extracapsular location was 28.2% (n=29) that should have been preserved (Figure 2D).
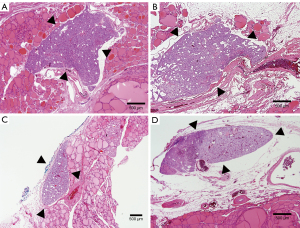
Table 2
| Histopathological locations | Values |
|---|---|
| Intracapsular location, n (%) | 74 (71.8) |
| Completely buried | 42 (40.8) |
| Partially buried | 15 (14.6) |
| Subcapsular | 17 (16.5) |
| Extracapsular location, n (%) | 29 (28.2) |
The clinical factors were compared between the partially buried and subcapsular location, versus the extracapsular location (Table 3). The extent of surgery, histopathology of thyroid, and extrathyroidal extension of cancer were considerable clinical factors, but none of them showed statistically significant difference.
Table 3
| Variables | Partially buried and subcapsular location (n=32) | Extra-capsular location (n=29) | P |
|---|---|---|---|
| Extent of surgery, n (%) | |||
| Hemi-thyroidectomy | 9 (28.1) | 9 (31.0) | 0.372† |
| Total thyroidectomy only | 18 (56.3) | 14 (48.3) | 0.233† |
| Total thyroidectomy with neck dissection | 5 (15.6) | 6 (20.7) | 0.295† |
| Histopathological features, n (%) | 0.095† | ||
| Benign | 7 (21.9) | 4 (13.8) | |
| Malignant | 25 (78.1) | 25 (86.2) | |
| Extra-thyroidal extension, n (%) | 13 (40.6) | 10 (34.5) | 0.241† |
†, Chi-squared test.
Discussion
In this study, the locations of parathyroid glands were classified as intracapsule and extracapsule because capsular dissection is the principle of thyroid surgery. Of the intracapsular parathyroid glands, the intrathyroidal parathyroid glands, which are completely buried in thyroid parenchyme, are almost impossible to find intraoperatively even with meticulous capsular dissection while subcapsular parathyroid gland is more likely to be found. However, even the most experienced surgeons receive pathologic reports indicating unintentionally removed intracapsular parathyroid glands despite the best efforts to save the parathyroid glands. Therefore, this study assumed that intracapsular other than intrathyroidal parathyroid glands may not routinely be visible to the naked eye depending on the size or location of them, and divided intracapsular location into completely buried in thyroid parenchyme, partially buried, and subcapsular location to offer more information on histopathologic location of parathyroid glands. The completely buried parathyroid gland is a definite anatomical risk factor of unintended removal (7,9). However, even partially buried parathyroid glands have a potential of unintended removal. We retrospectively examined the partially buried parathyroid glands which made it difficult to preserve them. In this study, fifteen unintentionally removed parathyroid glands (14.6%) which were partially buried were observed. This location might act with similar risk factor as the completely buried parathyroid glands because partially buried parathyroid glands cannot be easily seen during surgery by the naked eye. Therefore, it may have been classified as completely buried in the past studies (5,8). Since partially buried parathyroid gland can act as an inevitable risk factor of unintended parathyroidectomy under the naked eye, surgeons do not necessarily need to be embarrassed or be frustrated about the pathologic report of unintended parathyroidectomy, and thereby do not have to routinely perform an excessive manipulation for identification of parathyroid gland next time because it can increase direct trauma or disrupt blood supply on parathyroid glands (10,11). However, meticulous capsular dissection of thyroid glands is still crucial principle of thyroid surgery.
Although the frequent anatomical location of partially buried parathyroid glands was not identified in the pathologic report of this study, a few studies have provided information of anatomical location of subcapsular and intrathyroidal parathyroid glands. According to the previous cadaveric study, 87.5% were inferior parathyroid among the subcapsular parathyroid glands (5). In case of intrathyroidal parathyroid gland, there were more inferior parathyroid glands than superior parathyroid glands but the specific numerical values were not provided. Another study investigated the anatomical location of unintentionally removed parathyroid glands relative to the thyroid gland and found that the most of them were inferior parathyroid glands and they were located on the right side (12). According to the previous study of removal of parathyroid adenoma, three quarters of intrathyroidal parathyroid glands were inferior parathyroid glands, and it assumed that inferior parathyroid glands might have more chance to be entrapped in thyroid glands due to longer distance of migration (8).
Newly developed intraoperative visualizing technique may lower the chance of unintended parathyroidectomy. Recently, many studies have been reported for visualization and maintenance of the parathyroid glands in situ. The near-infrared fluorescence imaging technique with indocyanine green (ICG) could find out the location of the parathyroid gland during thyroid surgery based on the fact that the parathyroid glands had a higher fluorescence intensity than thyroid, lymph nodes or fat (13,14). Autofluorescence imaging using the natural emission of light by intrinsic fluorophores is an emerging non-invasive and safe technique to find the location of the parathyroid gland during surgery (15,16). Autofluorescence imaging allows surgeons to utilize high-quality fluorescence images of circulation including lymphatics and blood vessels during thyroid surgery (16). According to the study by Benmiloud et al., nearly two-thirds of identified parathyroid glands were detected by the near-infrared camera before visual identification, and the number of unintended removal of parathyroid glands was significantly lower in near-infrared autofluorescence group than in the standard-care group adopting conventional capsular dissection with visualization of parathyroid glands by the naked eye (17). Other studies reported similar results that the parathyroid glands covered by fibrofatty tissues were detected by near-infrared camera before visual identification in 77% to 93% of patients (18,19). There is a known limitation that the ability of near-infrared light to penetrate tissue is limited to a depth of 2 to 3 mm maximum and if parathyroid glands are located deeper than 3 mm, autofluorescence may not be detected (20). However, this limitation will not be a critical issue if surgeons perform a meticulous capsular dissection of thyroid gland and then shine near-infrared light on to the thyroid gland because the thin capsular propria covering partially buried parathyroid glands after capsular dissection does not exceed a few millimeters. Inspection of removed thyroid specimen with near-infrared light and subsequent autotransplantation of identified partially buried parathyroid can be another option to avoid unintended parathyroidectomy because autofluorescence of parathyroid glands maintain its emission for at least one hour after resection (21). As a result, partially buried parathyroid glands can have more chance to be saved with the help of near-infrared light compared to the intrathyroidal parathyroid glands because the depth of thyroid tissue covering the intrathyroidal parathyroid glands may exceed a few millimeters. With current conventional operative technique of thyroid surgery, it would be very challenging to preserve partially buried parathyroid glands and even subcapsular parathyroid glands. However, continued advances in visualizing technique may lower the chance of incidentally removed partially buried and subcapsular parathyroid glands in the future although further large randomized prospective studies need to be preceded to validate these techniques.
The clinical factors between the partially buried and subcapsular location, and extracapsular location of the parathyroid gland in unintended parathyroidectomy were compared in this study. The extent of surgery, histologic characteristics, and extrathyroidal extension of the cancer did not show significant differences between two groups. Extrathyroidal extension has been reported as a risk factor of unintended parathyroidectomy (22,23). The authors initially predicted that the subcapsular or partially buried parathyroid gland had a higher risk of unintended parathyroidectomy in cases with extrathyroidal extension of thyroid cancer because capsular dissection would be more difficult. However, the rates of extrathyroidal extension were not different between two groups in this study. In other words, partially buried and even subcapsular parathyroid themselves might be considered innate risk factors of unintended parathyroidectomy regardless of capsular dissection though more relevant research needs to be preceded.
This study has some limitations. First, the sample size was small. Second, the surgical anatomical locations of each incidentally removed intracapsular parathyroid glands were not provided due to the nature of retrospective study. Pathologic reports did not specify their anatomical locations such as superior or inferior and left or right.
Conclusions
This study is meaningful that a partially buried parathyroid gland may explain the possibility of an unintended parathyroidectomy despite the surgeon’s best effort with meticulous capsular dissection. In other words, a partially buried parathyroid gland can act as a risk factor for unintended parathyroidectomy comparable to intrathyroidal parathyroid gland. This study proposed to divide the classification of histopathologic location of parathyroid glands into extracapsule and intracapsule, and additionally divide intracapsular parathyroid gland into completely buried, subcapsular and partially buried. With this new classification, newly developed visualizing techniques may help to find more partially buried parathyroid glands that are likely to have been classified as completely buried in the past studies, and this process will be able to reduce unintended parathyroidectomy. However, apart from this, surgeons need to continue capsular dissection with the naked eye to preserve the subcapsular parathyroid glands.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at https://gs.amegroups.com/article/view/10.21037/gs-23-282/rc
Data Sharing Statement: Available at https://gs.amegroups.com/article/view/10.21037/gs-23-282/dss
Peer Review File: Available at https://gs.amegroups.com/article/view/10.21037/gs-23-282/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://gs.amegroups.com/article/view/10.21037/gs-23-282/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. This study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the Institutional Review Board of Korea University Guro Hospital (No. 2018GR0229) and individual consent for this retrospective analysis was waived.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Gourgiotis S, Moustafellos P, Dimopoulos N, et al. Inadvertent parathyroidectomy during thyroid surgery: the incidence of a complication of thyroidectomy. Langenbecks Arch Surg 2006;391:557-60. [Crossref] [PubMed]
- Page C, Strunski V. Parathyroid risk in total thyroidectomy for bilateral, benign, multinodular goitre: report of 351 surgical cases. J Laryngol Otol 2007;121:237-41. [Crossref] [PubMed]
- Lee NJ, Blakey JD, Bhuta S, et al. Unintentional parathyroidectomy during thyroidectomy. Laryngoscope 1999;109:1238-40. [Crossref] [PubMed]
- Praženica P, O’Driscoll K, Holy R. Incidental parathyroidectomy during thyroid surgery using capsular dissection technique. Otolaryngol Head Neck Surg 2014;150:754-61. [Crossref] [PubMed]
- Hojaij F, Vanderlei F, Plopper C, et al. Parathyroid gland anatomical distribution and relation to anthropometric and demographic parameters: a cadaveric study. Anat Sci Int 2011;86:204-12. [Crossref] [PubMed]
- Sakorafas GH, Stafyla V, Bramis C, et al. Incidental parathyroidectomy during thyroid surgery: an underappreciated complication of thyroidectomy. World J Surg 2005;29:1539-43. [Crossref] [PubMed]
- Sasson AR, Pingpank JF Jr, Wetherington RW, et al. Incidental parathyroidectomy during thyroid surgery does not cause transient symptomatic hypocalcemia. Arch Otolaryngol Head Neck Surg 2001;127:304-8. [Crossref] [PubMed]
- Mazeh H, Kouniavsky G, Schneider DF, et al. Intrathyroidal parathyroid glands: small, but mighty (a Napoleon phenomenon). Surgery 2012;152:1193-200. [Crossref] [PubMed]
- Erbil Y, Barbaros U, Ozbey N, et al. Risk factors of incidental parathyroidectomy after thyroidectomy for benign thyroid disorders. Int J Surg 2009;7:58-61. [Crossref] [PubMed]
- Puzziello A, Rosato L, Innaro N, et al. Hypocalcemia following thyroid surgery: incidence and risk factors. A longitudinal multicenter study comprising 2,631 patients. Endocrine 2014;47:537-42. [Crossref] [PubMed]
- Lang BH, Chan DT, Chow FC. Visualizing fewer parathyroid glands may be associated with lower hypoparathyroidism following total thyroidectomy. Langenbecks Arch Surg 2016;401:231-8. [Crossref] [PubMed]
- Sitges-Serra A, Gallego-Otaegui L, Suárez S, et al. Inadvertent parathyroidectomy during total thyroidectomy and central neck dissection for papillary thyroid carcinoma. Surgery 2017;161:712-9. [Crossref] [PubMed]
- Lavazza M, Liu X, Wu C, et al. Indocyanine green-enhanced fluorescence for assessing parathyroid perfusion during thyroidectomy. Gland Surg 2016;5:512-21. [Crossref] [PubMed]
- Zaidi N, Bucak E, Yazici P, et al. The feasibility of indocyanine green fluorescence imaging for identifying and assessing the perfusion of parathyroid glands during total thyroidectomy. J Surg Oncol 2016;113:775-8. [Crossref] [PubMed]
- Kim SW, Lee HS, Lee KD. Intraoperative real-time localization of parathyroid gland with near infrared fluorescence imaging. Gland Surg 2017;6:516-24. [Crossref] [PubMed]
- Ladurner R, Sommerey S, Arabi NA, et al. Intraoperative near-infrared autofluorescence imaging of parathyroid glands. Surg Endosc 2017;31:3140-5. [Crossref] [PubMed]
- Benmiloud F, Godiris-Petit G, Gras R, et al. Association of Autofluorescence-Based Detection of the Parathyroid Glands During Total Thyroidectomy With Postoperative Hypocalcemia Risk: Results of the PARAFLUO Multicenter Randomized Clinical Trial. JAMA Surg 2020;155:106-12. [Crossref] [PubMed]
- Kahramangil B, Dip F, Benmiloud F, et al. Detection of Parathyroid Autofluorescence Using Near-Infrared Imaging: A Multicenter Analysis of Concordance Between Different Surgeons. Ann Surg Oncol 2018;25:957-62. [Crossref] [PubMed]
- Kim SW, Lee HS, Ahn YC, et al. Near-Infrared Autofluorescence Image-Guided Parathyroid Gland Mapping in Thyroidectomy. J Am Coll Surg 2018;226:165-72. [Crossref] [PubMed]
- Wolf HW, Runkel N, Limberger K, et al. Near-infrared autofluorescence of the parathyroid glands during thyroidectomy for the prevention of hypoparathyroidism: a prospective randomized clinical trial. Langenbecks Arch Surg 2022;407:3031-8. [Crossref] [PubMed]
- De Leeuw F, Breuskin I, Abbaci M, et al. Intraoperative Near-infrared Imaging for Parathyroid Gland Identification by Auto-fluorescence: A Feasibility Study. World J Surg 2016;40:2131-8. [Crossref] [PubMed]
- Wang B, Du ZP, Qiu NC, et al. Application of carbon nanoparticles accelerates the rapid recovery of parathyroid function during thyroid carcinoma surgery with central lymph node dissection: A retrospective cohort study. Int J Surg 2016;36:164-9. [Crossref] [PubMed]
- Barrios L, Shafqat I, Alam U, et al. Incidental parathyroidectomy in thyroidectomy and central neck dissection. Surgery 2021;169:1145-51. [Crossref] [PubMed]


