Early intact PTH (iPTH) is an early predictor of postoperative hypocalcemia for a safer and earlier hospital discharge: an analysis on 260 total thyroidectomies
Introduction
Hypocalcemia is the most frequent complication after thyroidectomy: it can be classified in transient (less than 6 months) or permanent (more than 6 months) hypocalcemia (1).
Serum calcium levels are reliable only 48–72 hours after surgery (1), for this reason this often causes an unnecessary prolonged hospital stay (if not otherwise complicated) in normo-calcemic patients. Early intact PTH (iPTH) sampling has been indicated as a valid and early predictor of postoperative hypocalcemia (1).
However, there is no consensus about the use of such a parameter as a predictor for calcium levels. It has been showed that 6 hours post-operative iPTH has a sensitivity >95% and a specificity >90% in the diagnosis of hypocalcemia after thyroid surgery (2-7).
The purpose of this study is to assess the ability of iPTH in predicting postoperative hypocalcemia in order to obtain a safe and early hospital discharge.
Methods
For this study we analyzed 260 patients underwent total thyroidectomy or completion thyroidectomy with postoperative iPTH evaluation.
Exclusion criteria were only basal high iPTH values and chronic renal failure.
Thyroidectomy procedures have been performed from the same equipe, with a standard approach including parathyroids saving and Intra-operative Neuro-Monitoring (IONM). Energy based devices (LigaSureTM or Harmonic FocusTM) have been regularly used.
Lymphadenectomy of the central compartment was performed in case of evidence of malignancy in fine needle aspiration cytology (FNAC) of the thyroid nodule. Lateral compartment lymphadenectomy was performed when preoperative evidence of metastases in imaging or cytological examination.
The dosage of iPTH was performed by chemiluminescent immunometric method via the STAT-IntraOperative-Intact-PTH system (Future Diagnostics©). The preoperative calcium was assessed the day before the surgical operation. The blood samplings of the iPTH were performed from 3 to 6 hours after thyroidectomy. Moreover, the postoperative serum calcium level was dosed at 24 and 48 hours after thyroidectomy despite from the symptoms. All the symptomatic patients and asymptomatic patients with serum calcium <7.0 mg/dL, were treated via calcium gluconate intravenous injection.
Asymptomatic patients presenting serum calcium values between 7.0 and 8.0 mg/dL were treated during hospitalization (and after discharge) via oral therapy with calcium carbonate and calcitriol.
In the study the following variables were considered: age, sex, clinical diagnosis, obesity (BMI ≥30), comorbidities, previous neck surgery, preoperative therapy (antiplatelet agents, anticoagulants, Lugol solution, methimazole), type of surgery (total thyroidectomy, completion thyroidectomy), dissectors used (ultrasonic, bipolar), lymphadenectomy, post-operative complications (dysphonia, bleeding), reoperation and pathological diagnosis (benign or malignant).
The postoperative hospital stay was considered as the primary end-point and it was compared to the post-operative serum calcium (24 and/or 48 hours after surgery) and iPTH levels. In addition, serum calcium and iPTH were considered as secondary end-points in association with the other aforementioned considered variables.
Continuous variables were categorized according to the median value or the cut-offs suggested by the literature: for example for serum calcium level the cut-off value was 8.0 mg/dL and three iPTH cut-offs were tested in order to assess which was the best value (10.0, 15.0, and 20.0 pg/mL) (7-11).
The differences in the comparison between the variables and the end-points were assessed using non-parametric tests (χ2, Mann-Whitney test, Pearson correlation test), as appropriate.
The level of significance was considered at P<0.05. Statistical analysis were performed using the software SPSS® 20.0 for Windows®.
Results
Among the 260 patients, 205 were female (78.8%) and 55 male (21.2%), with a median age of 56 years (range, 18–84 years). Total thyroidectomy was performed in 251 patients (96.5%), and a completion thyroidectomy in 9 cases (3.5%).
Lymphadenectomy of the central neck compartment was performed in 13 patients (5.0%); lymphadenectomy of the lateral neck compartment in 2 patients (0.8%). In Table 1 the descriptive characteristics of the sample for any variables considered in the study are reported.
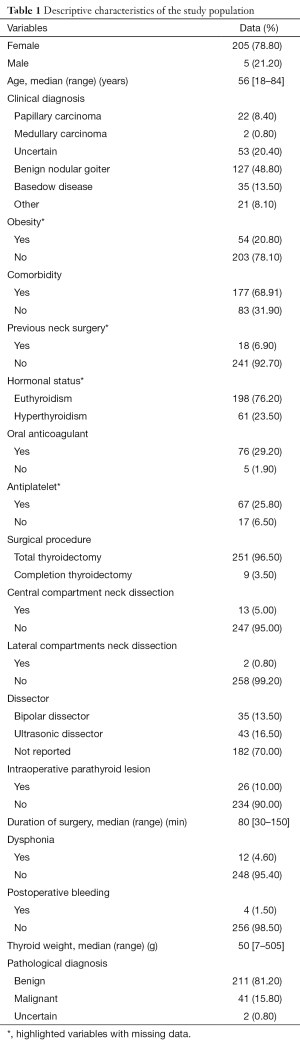
Full table
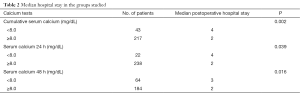
The postoperative hospital stay ranged between 1 and 36 days with a median of 2 days: 149 patients (57.3%) had a hospital stay <2 days, while 111 (42.7%) were hospitalized for more than 2 days after the surgical procedure. In the first group the median is 2 days while in the second group is 4 days.
The median preoperative calcium level for all the patients was 9.6 mg/dL (range, 8.0–11.0 mg/dL). The cumulative data about postoperative serum calcium had a median of 8.6 mg/dL (range, 7.0–11.0 mg/dL). Similarly, the serum calcium 24 hours after surgery had a median of 8.6 mg/dL (range, 7.0–11.0 mg/dL); the serum calcium level 48 hours after surgery showed a median of 8.5 mg/dL (range, 6.0–11.0 mg/dL). Patients presenting cumulative serum calcium <8.0 mg/dL were 43 (43/260, 16.5%), while those with serum calcium level ≥8.0 mg/dL were 217 (217/260, 83.5%). There were 22 patients with 24 hours postoperative serum calcium <8.0 mg/dL (22/260, 8.5%), and 238 patients presented serum calcium levels ≥8.0 mg/dL (238/260, 91.5%). Patients with 48 hours post-op serum calcium <8.0 mg/dL were 64 (64/248, 25.8%), while those with 48 hours post-op serum calcium ≥8.0 mg/dL were 184 (184/248, 74.2%).
The postoperative value of the median iPTH was 28.0 pg/mL ranging between 4.0 and 1,434.0 pg/mL.
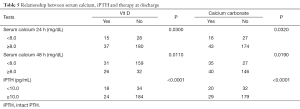
The median post-operative hospital stay has been compared in groups that had the cumulative values of serum calcium 24 and 48 hours after surgery ≥8.0 or <8.0 mg/dL (Table 2). Analyzing the correlation, via the Pearson-test, between serum calcium and iPTH no statistically significant linear correlation has been shown (r=0.026, P=0.68). Consequently, the association of serum calcium and iPTH has been further analyzed. The patients’ distribution in groups presenting serum calcium ≥8.0 or <8.0 mg/dL was investigated and compared to the iPTH values. The iPTH cut-off value was set at 10.0, 15.0, and 20.0 pg/mL (7-11).
Full table
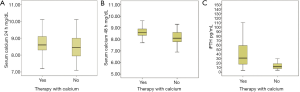
Even if there was the same level of statistical significance (Table 3), the iPTH cut-off value of 10.0 pg/mL was the most accurate (76.0%) and the most specific (83.0%) in predicting the post-operative serum calcium in comparison to the iPTH cut-off of 15.0 pg/mL (accuracy of 73% and a specificity of 75%) and to the iPTH cut-off of 20.0 pg/mL (accuracy of 67.0% and a specificity of 64.0%) (Figure 1).

Full table

Comparing the iPTH value (cut-off set at 10.0 pg/mL) with the different values of serum calcium respectively 24 and 48 hours after surgery, a statistically stronger association with the serum calcium levels 48 hours after surgery has been shown (Table 4).

Full table
Moreover, it was studied the correlation of serum calcium 24 and 48 hours after surgery and the iPTH values compared with the need of calcium carbonate and vitamin D therapy at hospital discharge (Table 5, Figure 2).
Full table
The other aforementioned variables have been finally compared to the secondary end-points in order to identify any potential differences to explain the different predictive values calculated for serum calcium and iPTH. We found that postoperative serum calcium level <8.0 mg/dL was strongly associated with variables different from those associated with iPTH <10.0 pg/mL. Particularly, a diagnosis of malignancy and the possibility of a central neck dissection were associated with a lower iPTH (13/38, P=0.049 and 7/45, P=0.002, respectively) without correlation with hypocalcemia.
Discussion
Early and safe hospital discharge in patients who underwent thyroidectomy can be defined as a postoperative hospital stay of <48 hours in order to exclude medical and surgical complications and to set the appropriate therapy. Among those, hypocalcemia is undoubtedly the most frequent event presenting an incidence between 0.3% and 43.0% for transient hypocalcemia and between 0 and 13.0% for permanent hypocalcemia (12).
In the present study, hypocalcemia was the most frequent observed complication with a global incidence of 8.8%. Other complications had an incidence of 1.5% for bleeding, and 3.1% for recurrent laryngeal nerve injury.
Bleeding and recurrent nerve injury usually occur in the immediate post-operative period, for this reason hypocalcemia it’s the only complication that affects the hospital discharge timing.
Serum calcium levels 24 hours after surgery is not considered a very reliable predictor for the need of calcium therapy at discharge (13). The assessment of serum calcium begins to have clinical significance and starts to be predictive of a safe discharge only at 48 hours after surgery (13-15). This value, when altered, seems to be associated with symptomatic hypocalcaemia and the need for post-discharge therapy (15).
In recent years, the identification of new early predictors of serum calcium levels 48 hours after surgery has become an important research topic.
Even if currently there is not an unanimous consensus on the use iPTH in routinely clinical settings (and in particular on its cut-off value and on its sampling timing) this test seems to be a promising solution to this predictive need (11,13,14).
The results of the present study confirmed the data reported in literature: the median hospital stay for patients with 48 hours serum calcium inferior to 8.0 mg/dL was 3 vs. 2 days for patients with 48 hours serum calcium ≥8.0 mg/dL (P=0.016). Moreover, 56.4% of patients with 48 hours post-op serum calcium <8.0 mg/dL received calcium carbonate versus 37.2% of those with 24 hours post-op serum calcium <8.0 mg/dL.
As reported in the literature, in our study the correlation of iPTH with hypocalcemia is significant starting from a few hours after surgery (11,14,16). This observation is consistent with the half-life of the iPTH (which is about 4 minutes).
The value of iPTH resulted more strongly associated with the serum calcium 48 hours after surgery than 24 hours after surgery (17,18).
Moreover the postoperative value <10 pg/mL is predictive of the need of calcium therapy at discharge. Hence, according to our results, the value of iPTH ≥10 pg/mL could be able to select those patients fit for a safe and early discharge (even in the first post-operative day in the absence of other complications).
Even if the sample of this study is wide, the main limitation of present paper is its retrospective nature and its results must be confirmed in prospective trials. However, this article confirmed that serum calcium levels 48 hours after surgery ≥8.0 mg/dL is associated with a discharge without the need for calcium therapy; moreover, iPTH ≥10 pg/mL 3–6 hours after surgery was strongly correlated to this possibility. Therefore, consistently with the literature results, it could be argued that the systematic use of the immediately postoperatively iPTH assay may avoid unnecessary extensions of hospitalization days with direct benefits for both the patient and, in terms of costs, for the institution.
In order to overcome the aforementioned limitations of this study we are designing the first prospective randomized trial, Early iPTH Assessment for a Safe and Early Discharge (EPHASED), with the aim to verify the possibilities of an early and safe discharge (after 12 hours after surgery) for patients who underwent thyroidectomy just on the basis of the iPTH values 1 hour after surgery.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: Project, research, development and ethical approval was obtained from the local Institutional Review Board (No. 182/INS/2016).
References
- Julián MT, Balibrea JM, Granada ML, et al. Intact parathyroid hormone measurement at 24 hours after thyroid surgery as predictor of parathyroid function at long term. Am J Surg 2013;206:783-9. [Crossref] [PubMed]
- Noordzij JP, Lee SL, Bernet VJ, et al. Early prediction of hypocalcemia after thyroidectomy using parathyroid hormone: an analysis of pooled individual patient data from nine observational studies. J Am Coll Surg 2007;205:748-54. [Crossref] [PubMed]
- Payne RJ, Hier MP, Tamilia M, et al. Same-day discharge after total thyroidectomy: the value of 6-hour serum parathyroid hormone and calcium levels. Head Neck 2005;27:1-7. [Crossref] [PubMed]
- Payne RJ, Tewfik MA, Hier MP, et al. Benefits resulting from 1- and 6-hour parathyroid hormone and calcium levels after thyroidectomy. Otolaryngol Head Neck Surg 2005;133:386-90. [Crossref] [PubMed]
- Payne RJ, Hier MP, Côté V, et al. Postoperative parathyroid hormone levels in conjunction with corrected calcium values as a predictor of post-thyroidectomy hypocalcemia: review of outcomes 1 year after the implementation of a new protocol. J Otolaryngol 2005;34:323-7. [Crossref] [PubMed]
- Graciano AJ, Chone CT, Fischer CA. Applicability of immediate, late or serial intact parathyroid hormone measurement following total thyroidectomy. Braz J Otorhinolaryngol 2012;78:78-82. [Crossref] [PubMed]
- Yano Y, Masaki C, Sugino K, et al. Serum intact parathyroid hormone level after total thyroidectomy or total thyroidectomy plus lymph node dissection for thyroid nodules: report from 296 surgical cases. Int J Endocrinol Metab 2012;10:594-8. [Crossref] [PubMed]
- McCullough M, Weber C, Leong C, et al. Safety, efficacy, and cost savings of single parathyroid hormone measurement for risk stratification after total thyroidectomy. Am Surg 2013;79:768-74. [PubMed]
- Cayo AK, Yen TW, Misustin SM, et al. Predicting the need for calcium and calcitriol supplementation after total thyroidectomy: results of a prospective, randomized study. Surgery 2012;152:1059-67. [Crossref] [PubMed]
- Costanzo M, Marziani A, Condorelli F, et al. Post-thyroidectomy hypocalcemic syndrome: predictive value of early PTH. Preliminary results. Ann Ital Chir 2010;81:301-5. [PubMed]
- Vanderlei FA, Vieira JG, Hojaij FC, et al. Parathyroid hormone: an early predictor of symptomatic hypocalcemia after total thyroidectomy. Arq Bras Endocrinol Metabol 2012;56:168-72. [Crossref] [PubMed]
- Randolph GW. Surgery of the Thyroid and Parathyroid Glands. 2nd ed. London: Elsevier Health Sciences, 2012.
- Kim JP, Park JJ, Son HY, et al. Effectiveness of an i-PTH measurement in predicting post thyroidectomy hypocalcemia: prospective controlled study. Yonsei Med J 2013;54:637-42. [Crossref] [PubMed]
- Lang BH, Yih PC, Ng KK. A prospective evaluation of quick intraoperative parathyroid hormone assay at the time of skin closure in predicting clinically relevant hypocalcemia after thyroidectomy. World J Surg 2012;36:1300-6. [Crossref] [PubMed]
- Herranz González-Botas J, Lourido Piedrahita D. Hypocalcaemia after total thyroidectomy: incidence, control and treatment. Acta Otorrinolaringol Esp 2013;64:102-7. [Crossref] [PubMed]
- Quiros RM, Pesce CE, Wilhelm SM, et al. Intraoperative parathyroid hormone levels in thyroid surgery are predictive of postoperative hypoparathyroidism and need for vitamin D supplementation. Am J Surg 2005;189:306-9. [Crossref] [PubMed]
- Wang TS, Roman SA, Sosa JA. Postoperative calcium supplementation in patients undergoing thyroidectomy. Curr Opin Oncol 2012;24:22-8. [Crossref] [PubMed]
- Chapman DB, French CC, Leng X, et al. Parathyroid hormone early percent change: an individualized approach to predict postthyroidectomy hypocalcemia. Am J Otolaryngol 2012;33:216-20. [Crossref] [PubMed]


