
The transverse upper gracilis flap for autologous breast reconstruction: patient satisfaction outcomes from a single centre experience
Highlight box
Key findings
• Transverse upper gracilis (TUG) flap has a failure rate of 3/57 and a satisfaction rate of 19/21 at the Royal Free Hospital.
What is known and what is new?
• The TUG flap is a reliable autologus option in patients where the deep inferior epigastric perforator flap is not suitable or available.
• This manuscript shows the safety of the TUG flap and adds patient reported outcomes.
What is the implication, and what should change now?
• The TUG flap may be considered as a primary option for candidates that fit the criteria owing to the favourable patient reported outcomes.
Introduction
Breast cancer is the commonest cancer affecting females, with an estimated 55,920 new cases per year in the UK (1). The high incidence of breast cancer and subsequent breast cancer surgery, causes flap options for autologous breast reconstruction an area of important research. The modern-day plastic surgeon is now equipped with an array of flap options. These include the novel lumbar perforator artery, transverse upper gracilis (TUG), profunda artery perforator (PAP) and the gold standard deep inferior epigastric perforator (DIEP) flap (2,3).
There are instances when patients are unsuitable for DIEP, owing to insufficient abdominal tissue, low body mass index (BMI), and potential damage to perforator vessels due to past abdominal surgery. In this scenario, particularly if patients also have small to moderate sized breasts, the TUG flap is increasingly being used as a safe alternative. The first UK national flap registry report 2019, shows TUG reconstruction as 1.67% (38/2,280) of breast reconstructions entered (4).
The TUG flap was first used by Yousif et al. in 1992 (5). However, since its development by Arnez et al. (6), there have been few studies investigating outcome-related data (7,8). It is increasingly recognized that patient reported outcome measures (PROMs) are an important way of assessing procedural outcomes (9). Thus, we carried out a retrospective review of TUG flap breast reconstructions performed at Royal Free Hospital and investigated patient satisfaction regarding the inner thigh donor site, breast appearance and psychosocial wellbeing. We present this article in accordance with the STROBE reporting checklist (available at https://gs.amegroups.com/article/view/10.21037/gs-23-93/rc).
Methods
We used Electronic Patient Records to review all TUG flap breast reconstructions between October 2010 and October 2021 at Royal Free Hospital. The study was registered as a clinical audit, and we followed the General Data Protection Regulation (GDPR) protocol throughout the data collection process. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by Royal Free audit committee and individual consent for this retrospective analysis was waived.
We contacted our patient cohort via telephone to investigate patient satisfaction, a validated approach reported in the literature (10). One patient died 6 years postoperatively (cause of death unrelated to flap) and thus was excluded from the PROMs investigation. We also issued telephone call follow-up reminders to maximize response rate.
We assessed patient satisfaction using a custom 31-item questionnaire, incorporating elements of the validated BODY-Q (11) and BREAST-Q (12) scoring scales (Appendix 1). Our questionnaire contained five sections. Section A assessed patient satisfaction with inner thighs (BODY-Q), investigating smoothness, muscle tone and appearance. Section B assessed patient satisfaction of body contouring scars (BODY-Q) investigating size, appearance, and texture. Sections C and D explored psychosocial well-being and overall breast satisfaction respectively (BREAST-Q), investigating acceptance of new breasts, clothing fitting and breast appearance. Finally, Section E included custom questions regarding overall patient satisfaction.
Statistical analysis
Scores from Sections A–D were totaled and converted in accordance with the Rash-Q protocol for final analysis. This was on a scale of 0–100, with higher number equating to better patient satisfaction outcomes. Quantitative data from Section E was analysed using Microsoft Excel and reported as percentages.
Operative technique
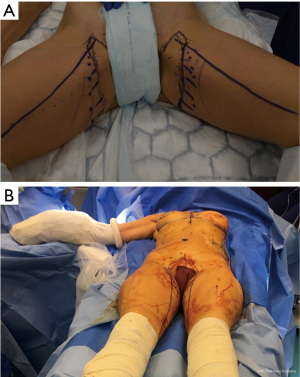
Pre-operatively the plastic surgeon positions the patient to lay supine (Figure 1A). The patient is then positioned with the knee flexed and thigh abducted to mark the crescent shaped flap needed to be raised (Figure 1B). The surgeon stands on the opposite side of the thigh from which the TUG is being raised and dissects superficially, cutting through muscular fascia with monopolar diathermy until the adductor longus is found. The loose areolar tissue between the gracilis and adductor longus can be released until the vascular pedicle is located. Large branches coming from the gracilis pedicle to adductor longus and magnus need to be controlled using ligaclips. It is important that the vascular pedicle of the gracilis is taken to its origin to reduce potential pedicle size mismatch with the internal mammary vessels. The pedicle length (mean length 6 cm in our series) can be maximized by making a window in the adductor longus and dividing the pedicle of the flap from its origin (Figure 2). Once the TUG flap has been raised it is commonly anastomosed with internal mammary artery and vein. It is important to consider a large internal mammary perforator as this may provide less of a vessel mismatch during end to end anastomosis. Our preference are the internal mammary vessels in the 4th interspace as it reduces the potential vessel mismatch. Internal mammary vessels allow for the anterograde and retrograde inset of the flap. In most cases we opted for Synovis couplers with a diameter of 1.5 mm. Furthermore, there is a low threshold for removing costal cartilage especially if the pedicle is short and in the event of stacked TUGs (Figure 3). Perfusion to the flap is checked using a Doppler probe and intraoperatively with indocyanine green. Regarding the reconstructed breast, the flap is folded and shaped (Figure 3). In the event of an immediate reconstruction, coning is preferred and an immediate nipple reconstruction. Postoperatively the patient will rest in a high-dependency unit for 3–4 days. The first 48 hours is a critical period where the flap is checked hourly for perfusion. Patients are expected to have returned to normal daily activities 6 weeks post-operation.

Results
Demographics
From 2010–2021, 57 TUG flaps were harvested in 36 patients for autologous reconstruction of 42 breasts, performed over 38 procedures. Follow-up ranged from 1 month to 11 years with a mean follow up of 3.8 years. Patient age ranged from 29–74 with an average of 49.5 years. Unilateral breast reconstruction using unilateral thigh as a donor site was performed in (19/38) procedures. In (15/38) procedures, both thighs were operated on at the same time as a donor site for unilateral breast reconstruction using two stacked TUG flaps. However, in (4/38) occasions, two TUG flaps were harvested from both thighs to be used for bilateral breast reconstruction. Most procedures were immediate reconstructions procedures (33/38) compared to delayed procedures (5/38) (Table 1).
Table 1
| Group | No. of procedures | Recipient | Donor | |||
|---|---|---|---|---|---|---|
| Breast | No. of procedures | Donor—thigh | No. of procedures | |||
| 1 | 19 | Unilateral breast reconstruction | 19 | Unilateral harvest | 19 | |
| 2 | 15 | Unilateral-stacked flap reconstruction | 15 | Bilateral harvest | 30 | |
| 3 | 4 | Bilateral breast reconstruction | 8 | Bilateral harvest | 8 | |
TUG, transverse upper gracilis.
Three out of fifty-seven flaps ended out with necrosis. In one patient, the flap showed partial necrosis and necrotic tissue was debrided until nicely bleeding. In another patient, total flap necrosis was noted, and exploration showed vascular thrombosis. The flap was removed, vessels were ligated, and the wound was washed out and closed over a drain. In the third case, the flap was not found perfused in the ward, the patient was taken to theatre, and pedicle exploration showed clotting of the artery and the two anastomosed veins. The flap was unsalvageable and then debrided. An anatomical implant was inserted subcutaneously, and acellular dermal matrix ADM was sutured around. Aside from breast hematoma (3/38), other complications included: infected hematoma/abscess of the donor site (1/38), dog ear of posterior thigh wound (2/38), wound dehiscence of the donor site (2/38), seroma infection (1/38), inclusion cyst of the reconstructed breast (1/38), contour deformity of the inner thigh (1/38), and necrosis of the medial mastectomy skin flap (1/38).
In our experience (17/36) patients had lipofilling, eight of them had more than one session. Also, (10/36) patients underwent revision procedures other than lipofilling; scar revision of the reconstructed breast (4/36), excision of dog ear of the donor thigh (2/36), excision of dog ear of the reconstructed breast (2/36), liposuction of the reconstructed breast to match the contralateral side (1/36), insertion of silicone implant in the previously reconstructed breast (1/36), scar revision of the donor site (1/36), and revision of the reconstructed nipple (1/36). Two patients had two revision procedures performed on the same session. Also, (14/42) breasts underwent nipple reconstructions, (4/14) of which were immediate in nature.
Twenty-one out of 35 patients responded to our telephone call survey (60% response rate). Out of the survey respondents 11/21 (52%) underwent unilateral procedures and 10/21 (48%) underwent bilateral procedures.
Patient satisfaction
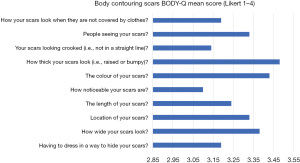
The BODY-Q appearance scale reported patient satisfaction in appraisal of thighs for all individual Likert scores (Figure 4) with a converted overall mean score of 76±27 points. In the appraisal of scars using the BODY-Q scale we reported all individual Likert scores (Figure 5) with a converted overall mean score of 71±20 points.
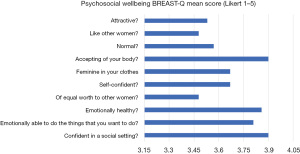
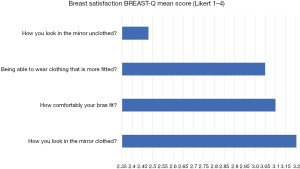
The BREAST-Q scale assessed psychosocial wellbeing for all individual Likert scores (Figure 6) with a converted overall mean score of 63±22 points. Also, we reported overall satisfaction with breasts for all individual Likert scores (Figure 7) with a converted overall mean score of 62±24 points.
In our custom-question Section E, 19/21 (90.5%) patients were satisfied with the outcome of the procedure. In addition, 17/21 (81%) in hindsight would opt for the TUG procedure again and the same number would recommend the TUG procedure to a friend or relative as a good treatment option.
Discussion
The TUG flap is used by a few centres in the UK and Europe as a second line treatment after the DIEP (7,8). The advantages of this procedure include consistent anatomy and simplicity in raising the flap, since no muscle dissection is required unlike in the DIEP or PAP flap. Moreover, this study reports excellent overall patient satisfaction (91%) suggesting that the TUG procedure is suitable for those who fit the criteria of low BMI and small to moderate sized breasts. However, the disadvantages are that limited flap volume can be harvested from the gracilis, the short pedicle and donor site complications.
In our experience, the TUG procedure had failure rates of 5.2% which is comparable with published literature (6). Difficulties which were encountered in our cohort included pedicle size mismatch compared to recipient vessels resulting in arterial insufficiency and thrombosis. This issue may have prevented Royal Free Hospital from achieving the lower reported failure rates of 2% (13). We attempted techniques to overcome vessel mismatch and to equalize the lumina. This included maximizing the pedicle length by making a window in the adductor longus and dividing the pedicle of the flap from its origin. Also, we utilised the internal mammary vessel in the fourth interspace to overcome the short pedicle length of the TUG flap and overcome the potential size mismatch during arterial anastomosis. Our preference for internal mammary vessels allows for the anterograde and retrograde onset of the flap and a low threshold for removing costal cartilage, especially if the pedicle is short and in the event of stacked TUGs. Further challenges were two cases that presented with unique anatomical variation. One patient had a double dominant gracilis pedicle, in this instance hematoma and abscess formed at the donor site. In addition, another patient had two pedicles of the Left TUG merging into one pedicle.
The lack of tissue harvested from TUG flaps resulted in slightly lower breast psycho-social wellbeing patient satisfaction scores (63 in our study) compared to that reported with DIEP patients (scores ranging 80–90) (14,15). Almost half our cohort required lipofilling to account for the limited amount of tissue that can be harvested from the inner thigh. Potential solutions for this include a stacked TUG flap which has been reported to have similar complication rate as single flap procedures (16). Additionally, the L-shaped modification of the TUG (17) and the diagonal upper gracilis (DUG) flap (18) may be adopted as viable methods to increase flap volume and as an extension patient breast satisfaction.
In contrast, the BODY-Q appearance scale reported excellent patient satisfaction in appraisal of inner thighs with an overall mean score of 76 points. We found our patient satisfaction regarding appraisal of inner thighs [−76] to be comparable to published TUG cohort scores (6,19). The discrete location of thigh scars in TUG flap in comparison to the visible abdominal scars left in DIEP flap is another advantage for female patient’s conscious of their appearance. Also, in our experience the TUG flap reconstruction preserved thigh strength post-raise, however there has been reported impact on abdominal strength with the DIEP (20). Ultimately, it is key to have multidisciplinary approach with early psychological input. If a patient has realistic expectations, their satisfaction following the surgery is likely to be higher (14).
This study has several limitations. Our study only had 36 patients with a 60% response rate which may not be representative of the entire patient cohort, resulting in response bias. Furthermore, the adverse impact of the coronavirus disease 2019 (COVID-19) pandemic was not a factor that was explored in this study. This is relevant as the COVID-19 pandemic has been reported to have negative psychological impact on breast cancer patients (21), which may have influenced patients when reporting BREAST-Q psychosocial wellbeing scores.
Conclusions
Overall, Royal Free Hospital reported excellent patient satisfaction outcomes with the TUG flap procedure for autologous breast reconstruction. Our study shows that the TUG flap is a primary candidate for those who fit the criteria. However, owing to almost 50% of patients requiring lipofilling, TUG modifications should be considered and patient expectations regarding breast appearance should be managed.
Acknowledgments
This work has been presented at the 11th Congress of World Society for Reconstructive Microsurgery.
Funding: None.
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at https://gs.amegroups.com/article/view/10.21037/gs-23-93/rc
Data Sharing Statement: Available at https://gs.amegroups.com/article/view/10.21037/gs-23-93/dss
Peer Review File: Available at https://gs.amegroups.com/article/view/10.21037/gs-23-93/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://gs.amegroups.com/article/view/10.21037/gs-23-93/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by Royal Free audit committee and individual consent for this retrospective analysis was waived.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Breast cancer statistics [Internet]. Cancer Research UK. 2021 [cited 13 December 2021]. Available online: https://www.cancerresearchuk.org/health-professional/cancer-statistics/statistics-by-cancer-type/breast-cancer
- Opsomer D, Stillaert F, Blondeel P, et al. The Lumbar Artery Perforator Flap in Autologous Breast Reconstruction: Initial Experience with 100 Cases. Plast Reconstr Surg 2018;142:1e-8e. [Crossref] [PubMed]
- Siegwart LC, Fischer S, Diehm YF, et al. The transverse musculocutaneous gracilis flap for autologous breast reconstruction: focus on donor site morbidity. Breast Cancer 2021;28:1273-82. [Crossref] [PubMed]
- Hazari A, Fowler C, Schache A, et al. The British Association of Plastic Reconstructive and Aesthetic Surgeons First UK National Flap Registry Report 2019 Mike Nugent FRCS (OMFS) BAOMS Dendrite Clinical Systems in collaboration with. Available online: https://bahno.org.uk/_userfiles/pages/files/uknfr_first_report_4dec_2019.pdf
- Yousif NJ, Matloub HS, Kolachalam R, et al. The transverse gracilis musculocutaneous flap. Ann Plast Surg 1992;29:482-90. [Crossref] [PubMed]
- Arnez ZM, Pogorelec D, Planinsek F, et al. Breast reconstruction by the free transverse gracilis (TUG) flap. Br J Plast Surg 2004;57:20-6. [Crossref] [PubMed]
- Locke MB, Zhong T, Mureau MA, et al. Tug 'O' war: challenges of transverse upper gracilis (TUG) myocutaneous free flap breast reconstruction. J Plast Reconstr Aesthet Surg 2012;65:1041-50. [Crossref] [PubMed]
- Pantelides NM, Jica RC, Patel NG, et al. Unilateral breast reconstruction using double transverse upper gracilis (TUG) flaps. J Plast Reconstr Aesthet Surg 2022;75:1164-70. [Crossref] [PubMed]
- Briffa N. The employment of Patient-Reported Outcome Measures to communicate the likely benefits of surgery. Patient Relat Outcome Meas 2018;9:263-6. [Crossref] [PubMed]
- Ng S, Kirkman M, Fisher J, et al. Establishing the acceptability of a brief patient reported outcome measure and feasibility of implementing it in a breast device registry - a qualitative study. J Patient Rep Outcomes 2019;3:63. [Crossref] [PubMed]
- Klassen D, Pusic D, Cano D. BODY-Q | Q-Portfolio - MEASURING WHAT MATTERS TO PATIENTS [Internet]. Qportfolio.org. 2021 [cited 13 December 2021]. Available online: https://qportfolio.org/body-q/
- Klassen D, Pusic D, Cano D. BREAST-Q | Breast Cancer - Q-Portfolio ADAPTABLE TO YOUR NEEDS [Internet]. Qportfolio.org. 2021 [cited 13 December 2021]. Available online: https://qportfolio.org/breast-q/breast-cancer/
- Siegwart LC, Bolbos A, Tapking C, et al. Safety and donor site morbidity of the transverse musculocutaneous gracilis (TMG) flap in autologous breast reconstruction-A systematic review and meta-analysis. J Surg Oncol 2021;124:492-509. [Crossref] [PubMed]
- Pusic AL, Klassen AF, Snell L, et al. Measuring and managing patient expectations for breast reconstruction: impact on quality of life and patient satisfaction. Expert Rev Pharmacoecon Outcomes Res 2012;12:149-58. [Crossref] [PubMed]
- Opsomer D, Vyncke T, Ryx M, et al. Comparing the Lumbar and SGAP Flaps to the DIEP Flap Using the BREAST-Q. Plast Reconstr Surg 2020;146:276e-82e. [Crossref] [PubMed]
- Haddock NT, Cho MJ, Teotia SS. Comparative Analysis of Single versus Stacked Free Flap Breast Reconstruction: A Single-Center Experience. Plast Reconstr Surg 2019;144:369e-377e. [Crossref] [PubMed]
- Berner J, Henton J, Blackburn A. The L-shaped modification of the transverse upper gracilis (TUG) flap. European Journal of Plastic Surgery 2020;43:837-42. [Crossref]
- Dayan E, Smith M, Sultan M, et al. The Diagonal Upper Gracilis (DUG) Flap. Plastic and Reconstructive Surgery 2013;132:33-4. [Crossref]
- Siegwart LC, Bolbos A, Haug VF, et al. Donor Site Morbidity in Unilateral and Bilateral Transverse Musculocutaneous Gracilis (TMG) Flap Breast Reconstruction: Sensation, Function, Aesthesis and Patient-Reported Outcomes. J Clin Med 2021;10:5066. [Crossref] [PubMed]
- Lee ZH, Chu CK, Asaad M, et al. Comparing Donor Site Morbidity for Autologous Breast Reconstruction: Thigh vs. Abdomen. Plast Reconstr Surg Glob Open 2022;10:e4215. [Crossref] [PubMed]
- Swainston J, Chapman B, Grunfeld EA, et al. COVID-19 Lockdown and Its Adverse Impact on Psychological Health in Breast Cancer. Front Psychol 2020;11:2033. [Crossref] [PubMed]




