
Radiation and free flaps: what is the optimal timing?
Introduction
Background
In light of the growing popularity and prevalence of autologous breast reconstruction, the optimal timing of radiation therapy has become an increasingly salient question. Post-mastectomy radiation therapy (PMRT) has been shown to decrease locoregional disease and improve overall survival rates, making it a critical component of breast cancer treatment (1,2). Criteria for PMRT are based on pathologic features and nodal involvement, including greater than four positive axillary lymph nodes, tumor size greater than five centimeters, stage T4 disease, and positive margins. Following the Early Breast Cancer Trialists’ Collaborative Group meta-analyses, which showed improved disease-free and overall survival after PMRT in women with one to three positive lymph nodes, these indications further expanded (3,4). The guidelines for PMRT continue to evolve as cancer care progresses towards less invasive surgical interventions and more refined risk-profiling.
Rationale and knowledge gap
The negative impact of radiation on tissue vascularity and cellularity is well-documented. Ionizing radiation triggers an inflammatory cascade that leads to fibrosis, vascular thrombosis, and atrophy of the skin and subcutaneous tissue (5,6). In the breast reconstruction patient, this often clinically presents as breast pain, delayed wound healing, contracture, asymmetry, and even reconstructive failure. Numerous studies have reproducibly demonstrated high complication rates in implant-based reconstruction with radiation (7-9), thus autologous tissue is widely favored in this setting. However, the literature regarding the effects of radiation on flap reconstruction remains mixed. Older studies have shown higher rates of late complications with immediate flap reconstruction followed by PMRT compared to delayed flap reconstruction after completion of radiation, whereas more recent reports demonstrate equivalent outcomes between immediate and delayed autologous flaps. As the ultimate goal of any autologous breast reconstruction is to create a soft, natural breast mound, it is imperative to understand how radiation impacts flap success both acutely and in the long-term.
Objective
Expanding indications for PMRT and increasing acceptance of immediate breast reconstruction have prompted a need to re-evaluate the optimal sequence. In this article, we set out to compare outcomes of free flap breast reconstruction when performed before or after radiotherapy, to better characterize each treatment algorithm.
Delayed reconstruction: overview and rationale
Historically, radiation following immediate autologous breast reconstruction has been believed to create suboptimal outcomes. Since early reports that radiation adversely affected cosmetic results, symmetry, and flap contracture, further clinical studies were conducted to illustrate these effects (10,11). Many experts therefore recommended delaying flaps until after PMRT to optimize not only aesthetic outcomes, but cancer treatment efficacy. Certain oncologic concerns previously supported delaying autologous reconstruction, such as avoiding delay in time to radiation initiation and avoiding compromise of radiation delivery to the chest wall by maintaining a planar field (12). Regardless, the oncologic safety of immediate reconstruction has now been reliably demonstrated. Numerous studies have shown equivalent locoregional recurrence and distant metastasis rates in patients undergoing radiotherapy with or without immediate reconstruction, suggesting there is no decrease in efficacy of radiation when reconstruction is performed (13,14).
As a bridge between delayed and immediate pathways, Kronowitz et al. proposed the concept of “delayed-immediate” breast reconstruction whereby a tissue expander is placed at the time of mastectomy while awaiting final pathologic results (15). If PMRT is deemed necessary, delayed reconstruction is pursued after completion of therapy. If patients do not require adjuvant radiation, definitive breast reconstruction is performed 2 weeks following expander placement. While this approach is intended to decrease complications associated with radiotherapy, it delays reconstruction in patients that do not need PMRT. It also commits all patients to a second surgery, with the associated increased healthcare costs, peri-operative risks, and personal costs of two recovery periods. Implementation of this protocol found lower rate of overall flap complications in delayed-immediate patients compared to standard delayed patients (24% vs. 38%); however, no comparison was made with immediate autologous reconstruction (16). Furthermore, approximately one-third of tissue expanders were lost in the delayed-immediate group, representing a significant source of additional morbidity.
Delayed reconstruction is often grouped as a monolithic category when contrasted with immediate reconstruction; however, timing of delayed reconstruction is not standardized, with various recommendations provided in the literature. Delayed-immediate reconstruction originally described waiting 3 months after completion of radiation to proceed with a flap (16), whereas other protocols have been reported ranging from several months to over a year. One study of flap reconstruction after PMRT separated patients based on completion of radiation greater or less than 12 months prior to reconstruction and found a significantly higher rate of total flap loss and re-operation in the less than 12 months cohort (17). In contrast, other studies found no statistically significant difference using a similar time cutoff, or when 6 months was used as the threshold (18,19). These findings may be consistent with the unpredictable and biphasic nature of radiation injury. Ionizing radiation triggers an acute inflammatory phase over days to weeks, then a delayed fibro-atrophic response that can extend from months to years after treatment (20). The variable extent and duration of radiation-induced damage may thus complicate establishing reliable cutoffs. The question of optimal timing thus persists within delayed reconstruction. Anecdotally, many surgeons, including the senior author, defer to clinical assessment of breast skin quality and laxity when deciding when to offer reconstruction in the post-radiation setting. This avoids re-operating on a site that is still acutely tight, inflamed, and predisposed to complications.
Immediate flap reconstruction: overview and rationale
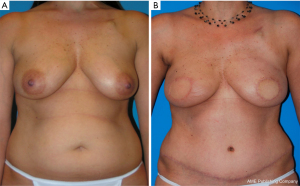
There are many well-described benefits to immediate breast reconstruction, across aesthetic, logistic, and psychosocial domains. Immediate reconstruction allows preservation of the skin envelope and breast footprint, creating a more natural-appearing breast. An immediate autologous flap can generally be buried with a small skin paddle that may be excised at a later date or used for nipple reconstruction, as opposed to the larger skin paddle required in delayed reconstruction once the skin has retracted and scarred. This difference in skin paddles is clearly demonstrated in Figure 1. Scar burden and unfavorable breast shape can thus initially be minimized when performing immediate reconstruction. The addition of radiotherapy has the potential to complicate these cosmetic advantages, as will be discussed in the next section comparing data on outcomes such as fat necrosis and flap shrinkage.

Importantly for patients, immediate reconstruction has been shown to enhance psychosocial well-being. In a large retrospective analysis of 577 patients who underwent either immediate or delayed reconstruction, the immediate group demonstrated higher scores for body image, self-esteem, and patient satisfaction (21). Other prospective studies following women years after mastectomy showed women with delayed reconstructions felt significantly higher levels of overall distress and depressive symptoms than those with immediate reconstructions, as well as less comfort with physical intimacy (22,23). Satisfaction with breast reconstruction was specifically evaluated in one prospective study using the BREAST-Q validated questionnaire. The authors compared patient-reported outcomes in 175 women undergoing delayed or immediate autologous reconstruction in the context of PMRT and found significantly lower pre-reconstruction scores for satisfaction with breast, psychosocial and sexual well-being in the delayed population (24). Notably, overall complication rates and satisfaction levels at 2 years post-operatively were similar between groups, suggesting breast aesthetics and quality of life were not compromised by flap radiation as evaluated from the patient’s perspective. By offering immediate flap reconstruction despite the need for PMRT, patients may obtain the same quality of life benefits and avoid waiting a prolonged period of time without a true breast mound.
Discussion: outcomes data
Multiple large studies and meta-analyses have been conducted in recent years to quantify the true effects of PMRT on autologous reconstruction. Reported complications encompass acute events such as flap loss or vessel thrombosis, and delayed events such as fat necrosis or flap contracture, as well as long-term patient-reported outcomes. While no standardized scale is applied across the literature, major complications are commonly defined as those requiring operative intervention, whereas minor complications resolve with conservative management, i.e., local wound dehiscence.
When evaluating aesthetics and volume changes, older reviews suggest worse outcomes when PMRT is given after flap reconstruction. An often-cited 2001 series compared immediate and delayed abdominal flaps with extended follow-up of 3 to 5 years and found a significantly greater incidence of late complications, consisting of volume loss, fat necrosis, and contracture of breast mounds, in the immediate reconstruction group (87.5% vs. 8.6%). Rates of flap loss or early vascular complications did not differ, but 28% of patients in the immediate cohort experienced flap distortion severe enough to require a second flap (25). Another study found flap shrinkage in approximately 30% of patients treated postoperatively with radiation, and 10% of patients went on to require a salvage procedure using an additional flap or an implant (26). A similar report documented fat necrosis or parenchymal fibrosis in 19.7% of flaps after radiation, necessitating revision surgeries (27). These types of findings led the authors to conclude that although immediate breast reconstruction with autologous tissue was a feasible option, it subjected patients to higher rates of fat necrosis and diminished aesthetics. Delayed flap reconstruction thus became standard practice for many plastic surgeons.
However, many of these studies consisted of small sample sizes and inconsistent outcome evaluations. One classic study of 625 abdominal-based flaps found irradiated flaps demonstrated a significantly higher rate of fat necrosis compared to non-radiated flaps (22.5% vs. 9.2%). However, the irradiated flaps were a far smaller sample size, only 40 patients, and there was no difference in re-operations for fat necrosis between the two groups, which raises the question of the clinical significance of the finding (28). Another large single-center review corroborated these findings, demonstrating a significantly higher incidence of volume loss and fat necrosis in flaps exposed to PMRT compared to non-radiated flaps, yet no difference in revision procedures (29). One small but interesting study used patients undergoing bilateral deep inferior epigastric perforator (DIEP) reconstruction with unilateral PMRT as internal controls to compare radiated vs. non-irradiated flap outcomes. There was no difference in fat necrosis between radiated or non-irradiated flaps, and aesthetic results based on photographic review were found to be satisfactory in all patients (30). These conclusions are consistent with our own clinical experience with immediate reconstruction and the quality of the cosmetic outcomes achieved (Figure 2).
More recently, several large subsequent studies have shown no impact of postoperative radiation on major complications in autologous reconstruction. A retrospective review of over 1,000 patients undergoing breast reconstruction with radiation delivered either before or after reconstruction (32) used multivariate analysis to show no significant difference in rates of major surgical complications and re-operations in autologous reconstruction patients who received postoperative radiotherapy (17.9% vs. 20.5%). Additional publications, including a prospective cohort study, found no differences in fat necrosis, wound healing, or need for surgical revisions for volume deficiency in hundreds of patients with either radiated or non-radiated free flap breast reconstructions (33,34). These findings were mirrored in a meta-analysis of 44 studies comparing complication rates between immediate and delayed breast reconstruction in the setting of PMRT. The authors demonstrated statistically equivalent rates of fat necrosis, flap loss, thrombosis, and infection (35). When specifically evaluating postoperative volume changes after unilateral DIEP reconstruction, measured as a volume ratio relative to the contralateral breast, a study using objective three-dimensional imaging found PMRT did not affect the volume ratio even at 12 months postoperatively (36).
Furthermore, concerns about delayed wound healing or increased surgical site complications due to postoperative radiation have not been borne out in the data. In a systematic review of outcomes associated with autologous breast reconstruction performed prior to or after chest wall radiation, complication rates were not significantly different (37). Pooled incidence of wound healing complications was 14% in flaps exposed to PMRT compared to 10% in flaps delayed after radiation, incidence of infection was 6% compared to 4%, incidence of hematoma was 1% compared 2%, and seroma rates were 4% in both groups. Furthermore, a follow-up paper to previous work by this senior author (Chang DW), providing an update on immediate vs. delayed autologous breast reconstruction paradigms, also found no difference in rates of surgical site infections, wound dehiscence, or fat necrosis (31). The number of revisions was in fact lower in the immediate reconstruction group than in the delayed group. Significantly lower volumes of fat grafting and fewer contralateral breast mastopexies were performed in the immediate cohort. This finding of fewer revisions has been reproduced in other studies (33,38) and is attributed to better baseline results obtained from immediate flap reconstruction. Importantly, wound complication incidence after immediate reconstruction has been shown to be relatively low and most complications minor in nature, so concerns about unreasonable delays in critical adjuvant oncologic treatments are not supported by the evidence (26,37,39).
Regarding microvascular complications, evidence initially suggested increased risk of thrombosis in delayed vs. immediate flap reconstruction, due to radiated recipient vessels. In a comparison of 226 radiated to 799 non-irradiated flaps, Fosnot et al. found prior radiation led to an increased rate of intraoperative microvascular complications (14.2% vs. 7.6%, P<0.003) and total vascular complications (17.3% vs. 9.6%, P<0.001), with statistical modeling showing radiotherapy was an independent risk factor (40). Rates of total flap loss, fat necrosis, and delayed wound healing in the radiation group were not significantly increased. Other investigations reported similar findings, showing increased likelihood of intraoperative vascular complications and need for arterial anastomotic revision (8% vs. 3%, P=0.04) in abdominal flaps transplanted to radiated vs. non-radiated chests (19). Such conclusions are difficult to translate however, without detailed information regarding radiation regimens and timing of surgery. Subsequent studies examining vascular complications have demonstrated no increased incidence of thrombosis or flap loss (24,31,37). A meta-analysis of observational studies identified no difference in early complication rates, or need for future revision surgery, when comparing immediate autologous breast reconstruction with and without PMRT (41).
Differences between findings in earlier vs. more recent studies may in part be attributed to advances in radiation techniques. Current methods use three-dimensional computed tomography planning, rather than the two-dimensional fields used previously. Variable beam angles, field sizes, and beam energies are implemented to optimize target penetration while minimizing dosage to surrounding tissues (42). Consequently, chest wall radiation damage is limited more than in the past, while maintaining oncologic efficacy. Nonetheless, radiation regimens vary widely by patient and by institution. One systematic review found many studies did not provide dosage details, and of those that did, regimens varied between 45 to 60 Gray given over a range of 3 to 6 weeks (43). Questions of internal mammary node radiation and bolus doses to the skin currently remain up to the discretion of each radiation oncologist. Some centers are also attempting to improve outcomes of reconstruction in early-stage breast cancer by using hypofractionation, which has shown promise in reducing the volume loss associated with standard PMRT (19,20). Subtle differences in dose delivery may have a meaningful impact on acute and late consequences of radiation damage.
Strengths and limitations
There are broad limitations to much of the evidence on this topic. Many studies involved limited sample sizes, single-surgeon experiences, and retrospective perspectives. High-quality data regarding the preferred sequencing of radiation and breast reconstruction are still lacking, partly due to the inherent lack of feasibility of patient randomization in this sensitive context. The heterogeneity between studies in methodology and reporting makes outcomes challenging to compare and precludes validation of any treatment strategy. For instance, “flap contracture” or “fat necrosis” is often defined without reproducible metrics and at various thresholds depending on the provider. The nuances of fat necrosis dimensions and symptomatology that are integral to the patient’s experience are lost with binary documentation of presence or absence.
Additionally, aesthetic outcomes are subjectively evaluated by surgeons, patients, or reviewers without standardization between studies, at times based solely on photographs. Statistical evaluation of cosmetic results between different grading scales consequently becomes impossible. Determining satisfactory or unsatisfactory results must take into account evaluations from patients themselves using validated questionnaires such as the BREAST-Q. Few existing studies of autologous breast reconstruction and PMRT apply validated patient-reported outcome measures.
These intrinsic methodological and statistical shortcomings consequently undermine the utility of the findings in current systematic reviews. Despite the amount of research on this subject, there is a limited amount of extractable data to pool. Aggregate information about radiation protocols and timing is also typically unavailable, and length of follow-up is limited across individual studies. Another inconsistency is that certain meta-analyses consider donor and recipient site complications together, although only recipient sites receive radiation. In the same vein, many reviews compare early wound healing complications in immediate vs. delayed groups, attributed to PMRT, however early complications may have occurred prior to the initiation of radiation in patients undergoing immediate flap reconstruction. Parenchymal changes of the breast flap are particularly of interest yet are non-uniformly reported in the literature. Few studies quantify or qualify the clinical severity of findings such as flap fibrosis, which can vary widely in its significance to patients and long-term consequences. Globally, clearer answers on this topic will require moving away from underpowered observational studies and towards multicenter prospective trials with objective, reproducible assessments.
Conclusions
In this review, we re-evaluate the paradigms recommending against immediate breast free flap reconstruction for patients who require PMRT. There are clear detrimental effects of radiation on soft tissue fibrosis, with unpredictable manifestations. Regardless, these possibilities must be weighed against the known adverse psychosocial effects of delaying breast reconstruction. The existing body of research suggests that, within limitations of heterogeneous reporting and variable radiation protocols, immediate free flap breast reconstruction in patients receiving PMRT can be performed without increased morbidity compared to delayed reconstruction.
It is this author’s opinion that immediate flap reconstruction followed by radiation can achieve satisfactory outcomes while avoiding the detrimental psychological effects of an absent breast and while maintaining cost efficacy. Recent evidence supports this as a successful reconstruction sequence that may reduce the number of surgical procedures required. A potentially higher risk of fat necrosis or flap contracture may persist but does not necessarily translate into clinical morbidity requiring re-operation.
Ultimately, the decision regarding surgical timing must be made individually between each patient and their surgeon. Patient satisfaction will be determined by a complex interplay between personal preferences, context, and objective outcomes, rather than by aggregate data. Many institution-specific variables should be considered as well, particularly the anticipated radiation regimen. Multidisciplinary discussion between the surgical oncologist, plastic surgeon, and radiation oncologist must reach a consensus about best practice for each patient’s unique pathology. When both immediate and delayed flaps are feasible, it is the role of the plastic surgeon to thoroughly discuss risks and benefits, guide the patient in their choices, and obtain maximally informed consent.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editors (Ketan M. Patel and Ara A. Salibian) for the series “Advances in Microsurgical Breast Reconstruction” published in Gland Surgery. The article has undergone external peer review.
Peer Review File: Available at https://gs.amegroups.com/article/view/10.21037/gs-23-154/prf
Conflicts of Interest: Both authors have completed the ICMJE uniform disclosure form (available at https://gs.amegroups.com/article/view/10.21037/gs-23-154/coif). The series “Advances in Microsurgical Breast Reconstruction” was commissioned by the editorial office without any funding or sponsorship. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Ragaz J, Jackson SM, Le N, et al. Adjuvant radiotherapy and chemotherapy in node-positive premenopausal women with breast cancer. N Engl J Med 1997;337:956-62. [Crossref] [PubMed]
- Recht A, Comen EA, Fine RE, et al. Postmastectomy Radiotherapy: An American Society of Clinical Oncology, American Society for Radiation Oncology, and Society of Surgical Oncology Focused Guideline Update. Ann Surg Oncol 2017;24:38-51. [Crossref] [PubMed]
- EBCTCG (Early Breast Cancer Trialists' Collaborative Group). Effect of radiotherapy after mastectomy and axillary surgery on 10-year recurrence and 20-year breast cancer mortality: meta-analysis of individual patient data for 8135 women in 22 randomised trials. Lancet 2014;383:2127-35. [Crossref] [PubMed]
- Donker M, van Tienhoven G, Straver ME, et al. Radiotherapy or surgery of the axilla after a positive sentinel node in breast cancer (EORTC 10981-22023 AMAROS): a randomised, multicentre, open-label, phase 3 non-inferiority trial. Lancet Oncol 2014;15:1303-10. [Crossref] [PubMed]
- Borger JH, Kemperman H, Smitt HS, et al. Dose and volume effects on fibrosis after breast conservation therapy. Int J Radiat Oncol Biol Phys 1994;30:1073-81. [Crossref] [PubMed]
- Davis AM, O'Sullivan B, Turcotte R, et al. Late radiation morbidity following randomization to preoperative versus postoperative radiotherapy in extremity soft tissue sarcoma. Radiother Oncol 2005;75:48-53. [Crossref] [PubMed]
- Ascherman JA, Hanasono MM, Newman MI, et al. Implant reconstruction in breast cancer patients treated with radiation therapy. Plast Reconstr Surg 2006;117:359-65. [Crossref] [PubMed]
- Cordeiro PG, Pusic AL, Disa JJ, et al. Irradiation after immediate tissue expander/implant breast reconstruction: outcomes, complications, aesthetic results, and satisfaction among 156 patients. Plast Reconstr Surg 2004;113:877-81. [Crossref] [PubMed]
- Kronowitz SJ, Robb GL. Radiation therapy and breast reconstruction: a critical review of the literature. Plast Reconstr Surg 2009;124:395-408. [Crossref] [PubMed]
- Spear SL, Ducic I, Low M, et al. The effect of radiation on pedicled TRAM flap breast reconstruction: outcomes and implications. Plast Reconstr Surg 2005;115:84-95. [Crossref] [PubMed]
- Rogers NE, Allen RJ. Radiation effects on breast reconstruction with the deep inferior epigastric perforator flap. Plast Reconstr Surg 2002;109:1919-24; discussion 1925-6. [Crossref] [PubMed]
- Nahabedian MY, Momen B. The impact of breast reconstruction on the oncologic efficacy of radiation therapy: a retrospective analysis. Ann Plast Surg 2008;60:244-50. [Crossref] [PubMed]
- Strålman K, Mollerup CL, Kristoffersen US, et al. Long-term outcome after mastectomy with immediate breast reconstruction. Acta Oncol 2008;47:704-8. [Crossref] [PubMed]
- Huang CJ, Hou MF, Lin SD, et al. Comparison of local recurrence and distant metastases between breast cancer patients after postmastectomy radiotherapy with and without immediate TRAM flap reconstruction. Plast Reconstr Surg 2006;118:1079-86. [Crossref] [PubMed]
- Kronowitz SJ, Hunt KK, Kuerer HM, et al. Delayed-immediate breast reconstruction. Plast Reconstr Surg 2004;113:1617-28. [Crossref] [PubMed]
- Kronowitz SJ, Lam C, Terefe W, et al. A multidisciplinary protocol for planned skin-preserving delayed breast reconstruction for patients with locally advanced breast cancer requiring postmastectomy radiation therapy: 3-year follow-up. Plast Reconstr Surg 2011;127:2154-66. [Crossref] [PubMed]
- Baumann DP, Crosby MA, Selber JC, et al. Optimal timing of delayed free lower abdominal flap breast reconstruction after postmastectomy radiation therapy. Plast Reconstr Surg 2011;127:1100-6. [Crossref] [PubMed]
- Momoh AO, Colakoglu S, de Blacam C, et al. Delayed autologous breast reconstruction after postmastectomy radiation therapy: is there an optimal time? Ann Plast Surg 2012;69:14-8. [Crossref] [PubMed]
- Fracol ME, Basta MN, Nelson JA, et al. Bilateral Free Flap Breast Reconstruction After Unilateral Radiation: Comparing Intraoperative Vascular Complications and Postoperative Outcomes in Radiated Versus Nonradiated Breasts. Ann Plast Surg 2016;76:311-4. [Crossref] [PubMed]
- Fajardo LF. Morphologic patterns of radiation injury. Front Radiat Ther Oncol 1989;23:75-84. [Crossref] [PubMed]
- Al-Ghazal SK, Sully L, Fallowfield L, et al. The psychological impact of immediate rather than delayed breast reconstruction. Eur J Surg Oncol 2000;26:17-9. [Crossref] [PubMed]
- Metcalfe KA, Zhong T, Narod SA, et al. A prospective study of mastectomy patients with and without delayed breast reconstruction: long-term psychosocial functioning in the breast cancer survivorship period. J Surg Oncol 2015;111:258-64. [Crossref] [PubMed]
- Metcalfe KA, Semple J, Quan ML, et al. Changes in psychosocial functioning 1 year after mastectomy alone, delayed breast reconstruction, or immediate breast reconstruction. Ann Surg Oncol 2012;19:233-41. [Crossref] [PubMed]
- Billig J, Jagsi R, Qi J, et al. Should Immediate Autologous Breast Reconstruction Be Considered in Women Who Require Postmastectomy Radiation Therapy? A Prospective Analysis of Outcomes. Plast Reconstr Surg 2017;139:1279-88. [Crossref] [PubMed]
- Tran NV, Chang DW, Gupta A, et al. Comparison of immediate and delayed free TRAM flap breast reconstruction in patients receiving postmastectomy radiation therapy. Plast Reconstr Surg 2001;108:78-82. [Crossref] [PubMed]
- Crisera CA, Chang EI, Da Lio AL, et al. Immediate free flap reconstruction for advanced-stage breast cancer: is it safe? Plast Reconstr Surg 2011;128:32-41. [Crossref] [PubMed]
- Albino FP, Koltz PF, Ling MN, et al. Irradiated autologous breast reconstructions: effects of patient factors and treatment variables. Plast Reconstr Surg 2010;126:12-6. [Crossref] [PubMed]
- Garvey PB, Clemens MW, Hoy AE, et al. Muscle-sparing TRAM flap does not protect breast reconstruction from postmastectomy radiation damage compared with the DIEP flap. Plast Reconstr Surg 2014;133:223-33. [Crossref] [PubMed]
- Mirzabeigi MN, Smartt JM, Nelson JA, et al. An assessment of the risks and benefits of immediate autologous breast reconstruction in patients undergoing postmastectomy radiation therapy. Ann Plast Surg 2013;71:149-55. [Crossref] [PubMed]
- Clarke-Pearson EM, Chadha M, Dayan E, et al. Comparison of irradiated versus nonirradiated DIEP flaps in patients undergoing immediate bilateral DIEP reconstruction with unilateral postmastectomy radiation therapy (PMRT). Ann Plast Surg 2013;71:250-4. [Crossref] [PubMed]
- Wu Young MY, Garza RM, Chang DW. Immediate versus delayed autologous breast reconstruction in patients undergoing post-mastectomy radiation therapy: A paradigm shift J Surg Oncol 2022;126:949-55. [Crossref] [PubMed]
- Berry T, Brooks S, Sydow N, et al. Complication rates of radiation on tissue expander and autologous tissue breast reconstruction. Ann Surg Oncol 2010;17:202-10. [Crossref] [PubMed]
- Chang EI, Liu TS, Festekjian JH, et al. Effects of radiation therapy for breast cancer based on type of free flap reconstruction. Plast Reconstr Surg 2013;131:1e-8e. [Crossref] [PubMed]
- Taghizadeh R, Moustaki M, Harris S, et al. Does post-mastectomy radiotherapy affect the outcome and prevalence of complications in immediate DIEP breast reconstruction? A prospective cohort study. J Plast Reconstr Aesthet Surg 2015;68:1379-85. [Crossref] [PubMed]
- Hershenhouse KS, Bick K, Shauly O, et al. Systematic review and meta-analysis of immediate versus delayed autologous breast reconstruction in the setting of post-mastectomy adjuvant radiation therapy J Plast Reconstr Aesthet Surg 2021;74:931-44. [Crossref] [PubMed]
- Lee MK, Park HY, Park JW, et al. Three-dimensional Volume Changes of the Reconstructed Breast Following DIEP Flap Breast Reconstruction. J Reconstr Microsurg 2023;39:427-34. [Crossref] [PubMed]
- Kelley BP, Ahmed R, Kidwell KM, et al. A systematic review of morbidity associated with autologous breast reconstruction before and after exposure to radiotherapy: are current practices ideal? Ann Surg Oncol 2014;21:1732-8. [Crossref] [PubMed]
- Heiman AJ, Gabbireddy SR, Kotamarti VS, et al. A Meta-Analysis of Autologous Microsurgical Breast Reconstruction and Timing of Adjuvant Radiation Therapy. J Reconstr Microsurg 2021;37:336-45. [Crossref] [PubMed]
- Foster RD, Hansen SL, Esserman LJ, et al. Safety of immediate transverse rectus abdominis myocutaneous breast reconstruction for patients with locally advanced disease. Arch Surg 2005;140:196-8; discussion 199-200. [Crossref] [PubMed]
- Fosnot J, Fischer JP, Smartt JM Jr, et al. Does previous chest wall irradiation increase vascular complications in free autologous breast reconstruction? Plast Reconstr Surg 2011;127:496-504. [Crossref] [PubMed]
- Schaverien MV, Macmillan RD, McCulley SJ. Is immediate autologous breast reconstruction with postoperative radiotherapy good practice?: a systematic review of the literature. J Plast Reconstr Aesthet Surg 2013;66:1637-51. [Crossref] [PubMed]
- Bazan J, DiCostanzo D, Kuhn K, et al. Likelihood of unacceptable normal tissue doses in breast cancer patients undergoing regional nodal irradiation in routine clinical practice. Pract Radiat Oncol 2017;7:154-60. [Crossref] [PubMed]
- Khajuria A, Prokopenko M, Greenfield M, et al. A Meta-analysis of Clinical, Patient-Reported Outcomes and Cost of DIEP versus Implant-based Breast Reconstruction. Plast Reconstr Surg Glob Open 2019;7:e2486. [Crossref] [PubMed]


