A rare cause of intermittent respiratory distress and epiphora in the newborn: congenital dacryocystocele
Introduction
Congenital dacryocystocele (CDC) is a malformation of the nasolacrimal unit which results from the obstruction of valve of Hasner in the lacrimal drainage system. Obstruction in the valve of Hasner is an anatomical barrier with an imperforate membrane at this level; it causes engorgement and swelling of the lacrimal sac. The swollen sac and nasolacrimal ductus leads to functional sac-canalicular junction obstruction (1). Secondary dacryocystitis may develop (2).
The common presenting symptoms of CDC are enlarged bluish cystic lesion around the medial canthal area, epiphora and high tear meniscus height at birth. In the rare cases of bilateral nasal involvement the patient may have respiratory distress needing urgent surgical manipulation (2).
In this case report; we presented a 2-week-old newborn with bilateral CDC with intermittent respiratory distress.
Case presentation
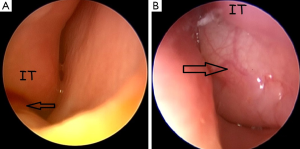
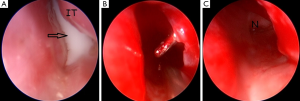
Two-week-old new born was admitted to our tertiary center with the complaint of bilateral bluish swelling in the medial canthal area and bilateral lachrymation. In her physical examination, there was a 1 cm blue colored swelling in the left side and 0.5 cm in the right side. There was no tenderness on palpation or infection signs such as hyperemia or fluctuation. Her parents claimed respiratory difficulty during feeding and sleeping. There were no features of syndromic or non-syndromic congenital anomalies or respiratory difficulty such as chest retraction. With the preliminary diagnosis of CDC, initially, conservative treatment option such as sac massage was advised to parents. On the first week follow up, right side swelling totally resolved whereas swelling of the left medial canthal region remained with tenderness on palpation and an erythema (Figure 1). Chest retraction during feeding was also seen. Under general anesthesia, endoscopic evaluation of bilateral nasal cavities and inferior meatus with a 0°, 2.7 mm endoscope revealed a small intranasal cyst in the right inferior meatus (Figure 2A) and a large one in the left side (Figure 2B). With a Bowman OO probe a successful probing on the right side could be done. The medial wall of the right side intranasal cyst was gently removed for prevention of the restenosis. For the left side; firstly an endoscopic incision was made on the wall of the cyst and pus discharge was seen from the cyst (Figure 3A). After marsupialization of the cyst with removal of the medial wall, successful probing with the Bowman OO probe could be achieved (Figure 3B). Left nasal passage was seen to be maintained after marsupialization (Figure 3C). In the postoperative period amoxicilline-clavulanic acid 200 mg (Augmentin 200 mg®-Glaxo Smith Kline drug) half dosage twice a day by oral route was administered for 10 days. The patient did well in the postoperative period without any complications. The swelling in the left medial canthal region, epiphora and respiratory difficulty during feeding completely resolved on the first week and sixth month control.
Discussion
In the embryogenesis of nasolacrimal system, at 10th week of gestation, a lumen in the lacrimal cord occurs with the cavitation of inferior meatal lamina which will form the valve of Hasner. Canalization of the lacrimal cord through the valve of Hasner at the sixth month of gestation is the last portion of the nasolacrimal system that will be patent during embryogenesis. If this fails, a membranous barrier forms at the level of the valve of Hasner (1). In this simple nasolacrimal obstruction, the system is blocked at a single point at the valve of Hasner, which is known as the congenital nasolacrimal duct obstruction. If there exists a second obstruction point at the level of valve of Rosenmuller secondary to engorgement in the lacrimal sac, CDC occurs. CDC occurs in only 0.1% of cases with congenital nasolacrimal duct obstruction (3,4). Classically, the main difference is the medial canthal region mass between the CDC and the congenital nasolacrimal duct obstruction (5), whereas rarely CDC can also present with only intranasal cyst without periorbital mass which makes the diagnosis difficult (4). The terms amniotocele, amniocele, dacryocele or mucocele are also used as synonyms of CDC (6). Most of the cases are unilateral, bilateral CDCs occur in 12–25% of cases. There is a female predominance due to the narrower nasolacrimal ducts in females (2,5,6).
Common presenting symptoms of CDC include mass in the medial canthal region and epiphora. Secondary dacryocystitis may occur (1). Pus extraction after incision of the cyst wall also shows secondary infection for our case. Rare secondary complications of CDC include anisometric amblyopia due to induced corneal astigmatism, and permanent canthal asymmetry due to chronic lacrimal distension (5). When the CDC has an intranasal extension with a mucocele, nasal symptoms can also occur. The exact incidence of intranasal extension or concomitant nasal mucocele in unilateral or bilateral CDC cases is unknown due to the scarcity of case reports and difficulty of an endoscopic examination in the newborn, but intranasal cyst can accomplish CDC in up to 80% of cases presented (7). The other factor preventing the prediction of intranasal cyst incidence for CDC cases is that most of the patients are primarily treated by an ophthalmologist, otolaryngologists are the ones that see the patients in the operating theatre (6). For our case, although the right side CDC resolved with conservative treatment, there was also a small intranasal cyst in the right inferior meatus. For bilateral cases, with intranasal extension life threatening respiratory distress can occur, since the infants are obligatory nasal breathers in the first 3 weeks of life (2). Kim et al. (2), Shashy et al. (5), Yohendran et al. (6), Leonard et al. (8), Trehan et al. (9), Hepler et al. (10), Jin et al. (11), Lecavalier et al. (12), Durmaz et al. (13) and Rogister et al. (14) presented cases of bilateral CDCs causing respiratory distress in the newborn. For patients with unilateral CDC and nasal extension, feeding difficulties, sleep disturbances and intermittent respiratory distress due to vascular congestion of the contralateral side during physiological nasal cycle can occur (8). Our case was a bilateral CDC with intranasal extension, but since the right side was affected minimally with a small intranasal cyst, respiratory distress occurred intermittently mostly during feeding and sleep.
Differential diagnosis of respiratory distress in the newborn is broad including congenital malformations such as choanal atresia, meningo-encephalocele, dermoid cyst, Thornwaldt cyst, pyriform aperture stenosis, tumoral lesions such as glioma, craniopharyngioma, and edema of the nasal mucosa (8). CDC with intranasal cyst, however, is typically not considered as a primary cause of respiratory distress in the newborn (4). Our case shows the importance of nasal endoscopic examination for newborns with respiratory distress and medial canthal region mass. For the differential diagnosis of CDC with intranasal extension, other paranasal lesions such as nasal encephalocele, dermoid, hemangioma, nasal glioma, lymphangioma, heterotrophic brain must be considered in the differential diagnosis (5,6). To differentiate CDC with intranasal mucocele from meningocele or encephalocele clinically, it is possible to pass a nasal endoscope medial to a nasolacrimal duct cyst, which is not possible in case of a meningocele or encephalocele (8). Ultrasonography is an inexpensive and easily available imaging method for initial imaging method of CDC cases. It can distinguish the cystic lesion from the vascular ones. Computerized tomography and magnetic resonance imaging studies can show the potential intracranial extension in case of a meningocele or encephalocele. Although the imaging techniques are helpful in narrowing the differential diagnosis, performing them in all cases is not mandatory, they can be adjusted when there is a suspicion in the preliminary diagnosis (5).
There is no globally accepted treatment algorithm for all CDC cases. Conservative methods such as external sac massage can help drainage of the cyst (1). However, recurrence or dacryocystitis can occur up to >20% of cases that are treated with these treatment modalities (5). During sac massage, rupture of the cyst into the nasal cavity through valve of Hasner mostly resolves the pathology, whereas if the cyst ruptures to the common canaliculi, cyst contents flow through the puncta and may cause a secondary dacryocystitis (7). Generally, the main indications for surgical treatment of CDC cases are concomitant infection or respiratory distress due to bilateral nasal involvement and unresponsiveness to conservative treatment options (8). However, Mimura et al. (7) presented the success of conservative management in the treatment of CDC cases even with intranasal involvement and dacryocystitis, they advised surgical treatment for only patients with respiratory distress. On the other hands, Kuboi et al. (4) presented a bilateral CDC case causing severe respiratory distress successfully treated with nasal mask nCPAP without surgical intervention. They emphasized that if CDC does not have infection signs, nCPAP can be used in the treatment even with respiratory distress. Our case demonstrates the importance of surgical intervention for CDC cases showing both signs of infection and respiratory distress. In the contemporary surgical management of CDC cases with intranasal cyst, two main surgical options are present: marsupialization of the intranasal cyst with nasal endoscopy, and combined endoscopic marsupialization with probing (8). Blind probing is no longer advised, since it can fail to perforate the wall of the intranasal cyst, or restenosis in the perforation site can occur (5). Endoscopic marsupialization decompresses the system distally, allowing the drainage of the retained fluid. Combined technique, as performed in our case, both supply decompression of the sac and continuity of the nasolacrimal system and it is the treatment of choice for most CDC cases with intranasal cysts (5,8). For our case, although the right site CDC recovered with conservative treatment, there was still a small intranasal cyst during endoscopic evaluation. To prevent restenosis, we also performed marsupialization of the right side cyst.
In conclusion, congenital dacryocystoceles are rare nasolacrimal anomalies. Since the exact incidence of the concomitant intranasal cysts is not known, the role of otolaryngologists in their treatment should be considered. If the endoscopic examination is not performed, simple probing may fail. Marsupialization of the intranasal cyst is mandatory not only for prevention of recurrences, but also for treating the respiratory distress. Otolaryngologist and ophthalmologists must be in contact with each other in the preoperative, intraoperative and follow-up period of these rare anomalies.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the parents of the patient for publication of this case report and any accompanying images.
References
- Cavazza S, Laffi GL, Lodi L, et al. Congenital dacryocystocele: diagnosis and treatment. Acta Otorhinolaryngol Ital 2008;28:298-301. [PubMed]
- Kim H, Park J, Jang J, et al. Urgent bilateral endoscopic marsupialization for respiratory distress due to bilateral dacryocystitis in a newborn. J Craniofac Surg 2014;25:e292-3. [Crossref] [PubMed]
- Başal Y, Akcan AB, Polat YD, et al. Rarely Seen Nasal Congenital Problems Causing Neonatal Upper Respiratory Obstruction: A Case Series. Pediatr Rep 2016;8:6456. [Crossref] [PubMed]
- Kuboi T, Okazaki K, Kusaka T, et al. Congenital dacryocystoceles controlled by nCPAP via nasal mask in a neonate. Pediatr Int 2015;57:475-7. [Crossref] [PubMed]
- Shashy RG, Durairaj VD, Holmes JM, et al. Congenital dacryocystocele associated with intranasal cysts: diagnosis and management. Laryngoscope 2003;113:37-40. [Crossref] [PubMed]
- Yohendran J, Wignall AC, Beckenham EJ. Bilateral congenital dacryocystocoeles with concurrent intranasal mucocoeles causing respiratory distress in a neonate. Asian J Surg 2006;29:109-11. [Crossref] [PubMed]
- Mimura M, Ueki M, Oku H, et al. Process of spontaneous resolution in the conservative management of congenital dacryocystocele. Clin Ophthalmol 2014;8:465-9. [Crossref] [PubMed]
- Leonard DS, O'Keefe M, Rowley H, et al. Neonatal respiratory distress secondary to bilateral intranasal dacryocystocoeles. Int J Pediatr Otorhinolaryngol 2008;72:1873-7. [Crossref] [PubMed]
- Trehan I, Turpin BK. Neonatal respiratory distress due to bilateral dacrocystoceles. J Pediatr 2008;153:438. [Crossref] [PubMed]
- Hepler KM, Woodson GE, Kearns DB. Respiratory distress in the neonate. Sequela of a congenital dacryocystocele. Arch Otolaryngol Head Neck Surg 1995;121:1423-5. [Crossref] [PubMed]
- Jin HR, Shin SO. Endoscopic marsupialization of bilateral lacrimal sac mucoceles with nasolacrimal duct cysts. Auris Nasus Larynx 1999;26:441-5. [Crossref] [PubMed]
- Lecavalier M, Nguyen LH. Bilateral dacryocystoceles as a rare cause of neonatal respiratory distress: report of 2 cases. Ear Nose Throat J 2014;93:E26-8. [PubMed]
- Durmaz A, Yildizoğlu Ü, Arslan F, et al. Bilateral dacryocystocele with an intranasal cyst as the cause of respiratory distress in a newborn. B-ENT 2016;12:23-7. [PubMed]
- Rogister F, Goffart Y, Daele J. Management of congenital dacryocystocele: report of 3 clinical cases. B-ENT 2016;12:83-8. [PubMed]



