
Completion thyroidectomy and lateral neck dissection revealed adhesions in the lateral neck compartment after gasless transaxillary endoscopic thyroidectomy: a case report
Introduction
Several alternative surgical techniques for the thyroid gland have been developed due to technological progress, both robotic and endoscopic with either a cervical or a remote-access approach (1). Endoscopic and robotic thyroidectomy is effective and safe surgical option for thyroid surgery while providing satisfactory cosmetic results (2). Unilateral transaxillary access is one of the most widely used method among the various robotic approaches (3). The da Vinci system is account for a prolonged surgical duration and a higher economic cost. Thus, gasless transaxillary endoscopic thyroidectomy has also been developed without robotic assistance (4). The transaxillary procedure is very different from the traditional open procedure. The anterior neck area was dissected through the anterior surface of the pectoralis major muscle, the sternocleidomastoid muscle (SCM) was dissected longitudinally between the sternal head and clavicular head, the strap muscles are dissected laterally, and the omohyoid muscle and internal jugular vein (IJV) were also exposed. Exposure of the lateral neck compartment, especially exposure of the IJV, causes difficulties for possible future lateral neck dissection (LND) due to disease recurrence and insufficient preoperational evaluation. Here, we present a patient who previously underwent gasless transaxillary endoscopic lobectomy with ipsilateral central neck dissection who underwent open completion thyroidectomy and LND (reoperation) in our center. We present the following case in accordance with the CARE reporting checklist (available at https://gs.amegroups.com/article/view/10.21037/gs-22-299/rc).
Case presentation
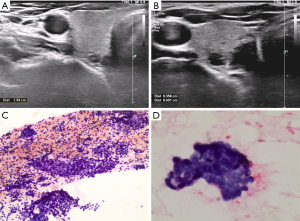
A 51-year-old female was diagnosed with thyroid nodules (4×3.6 and 3.3×3.1 mm in the right lobe) by ultrasound [the Thyroid Imaging Reporting and Data System (TI-RADS) scores were both 4a, Figure 1A,1B] without abnormal lymph nodes in the central and lateral neck compartments. Hence, a computed tomography (CT) examination and further evaluation of the neck lymph nodes was not performed before surgery. Fine needle aspiration (FNA) cytology revealed that the nodule was malignant (Bethesda VI, Figure 1C,1D). There was no history of surgery or underlying disease. Routine preoperative evaluations, such as electrocardiography (ECG), chest radiography and other laboratory tests, were normal. She was admitted for gasless transaxillary endoscopic lobectomy. This study was approved by the institutional review board of Xiangya Hospital, Central South University (No. 202011960). All procedures performed in this study were in accordance with the Declaration of Helsinki (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
This patient underwent gasless transaxillary endoscopic lobectomy on the 3rd day of hospitalization. After general anesthesia, the patient was placed in a supine position and the lesion side limb extended 90 degrees. A 4 cm length incision and an accessary 5 mm incision was made as described by our team. The route to the anterior neck area was dissected and the SCM was exposed (5). Then the strap muscles were dissected laterally, the omohyoid muscle and IJV were exposed and the retractor was placed beneath the straps muscle to finish working space making (5). The right lobe and isthmus of the thyroid gland were simultaneously removed for intraoperative frozen section biopsies (FSBs). The results suggested papillary thyroid carcinoma. Unilateral central compartment lymph node clearance was conducted. The postoperative pathological results were consistent with the FSBs results (two malignant nodules) and did not show lymph node metastasis (0/5). Postoperative recovery was uneventful. She was discharged home on the second day postoperatively.
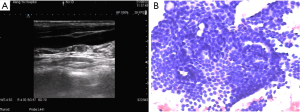
She received a dose of 50 µg L-T4 after surgery. Follow-up one month later revealed a thyroid stimulating hormone (TSH) level of 0.763 mIU/L, a Tg level of 86.02 ng/mL and normal FT3, FT4 and TgAb levels. Ultrasound tests were not routinely performed at the one-month visit in our center. She did not participate in the originally planned follow-up at the 3- and 6-month visits. At the one-year visit, an ultrasound test revealed enlarged and suspicious malignant lymph nodes in levels III and IV of the lateral neck compartments (Figure 2A). Lymph node FNA washout revealed a Tg level of >500 ng/mL. The CT examination results also revealed enlarged neck lymph nodes in the right lateral neck compartment. FNA cytology revealed metastatic foci (Figure 2B). Therefore, she was scheduled for a completion thyroidectomy and selective LND (right side).
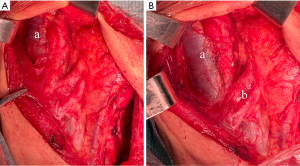
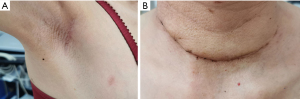
A 10 cm extended cervical collar incision was made. After completion thyroidectomy, the skin flap was applied to the anterior edge of the trapezius posteriorly and to the hyoid bone superiorly. The residual central compartment (left side) and modified LND, including sublevels IIA, III, IV, and VB, were applied. The medial border of the SCM was dissected, and then the SCM was pulled apart and oriented laterally to expose the omohyoid muscle and IJV. The surface of IJV was significantly adhered to the surrounding fibroadipose tissue (Figure 3A), and the omohyoid muscle was adhered to the IJV (Figure 3B). The IJV was carefully dissected, revealing that the adhesions were only involved in the segments of the IJV located in level III. The adhesions of the IJV and omohyoid muscle did not affect the dissection of level II & IV lymph nodes and affect only the dissection of the medial margin of level III lymph nodes. Important anatomical structures, including the spinal accessory nerve (SAN), brachial nerve, phrenic nerve, cervical plexus nerve, and transverse cervical artery were exposed and preserved. No complications were observed, with a parathyroid hormone (PTH) level of 18.43 pg/mL and a Ca2+ level of 2.2 mmol/L the day after surgery. She was discharged home on the third day postoperatively. The postoperative pathological results showed lateral lymph node metastasis in levels IIA (0/7), III (3/10), IV (2/8) and VB (0/6). She received a dose of 100 µg L-T4 after surgery. Follow-up one month later revealed a TSH level of 0.068 mIU/L and a Tg level of <0.04 ng/mL. Both axillary and neck incisions healed well (Figure 4).
Discussion
Remote-access thyroid surgery techniques have successfully avoided an anterior neck incision by moving the cutaneous incision to a less obvious locations (6). Extracervical techniques have shown considerable development with approaches that have included breast, transaxillary, transoral and postauricular routes (7). An increasing number of studies have provided strong evidence that endoscopic approaches are equally safe and effective treatments with additionally better cosmetic satisfaction for thyroid cancer when compared to open procedures (8). Nevertheless, it should be kept in mind that remote-access thyroidectomy only play a role in a small proportion of patients who meet the strict selection criteria. These approaches require an additional level of expertise and should therefore be performed by surgeons performing large numbers of thyroid and endoscopic procedures (9). Transaxillary, bilateral axillo-breast approach (BABA) robotic, transoral, and endoscopic total mammary areola approaches have been reported to achieve endoscopic thyroidectomy in our center (4,10,11). We further evaluated the safety and effectiveness of these endoscopic approaches compared with conventional approaches and showed that endoscopic procedures were similar to conventional procedures in safety, efficacy, and tumor recurrence but with better cosmetic results and higher patient satisfaction rates regarding quality of life.
Endoscopic thyroidectomy also yields new problems and complications. For instance, mental nerve injury is a characteristic complication of transoral surgery (12). A modified approach that dissected of the mental nerve via the oral approach is safe and feasible as reported (13). Tract hemorrhage and recurrence are other newly introduced and rare complications of endoscopic procedures (14,15). New complications arising from the transaxillary approach have also been observed, such as IJV and external jugular vein injury, which rarely occur in conventional approaches (without LND). Notably, almost all patients who underwent gasless endoscopic thyroidectomy in our center complained of paraesthesia and stiffness around the anterior chest area and SCM one week after surgery. However, discomfort was relieved over time, and the results were acceptable (4).
As reported, the most common sites of recurrence were the central and lateral compartments, ipsilateral to the largest thyroid tumor (16). LND-related complications were observed more frequently following reoperative LND (IJV injury, hematoma and lymphatic leakage) than following primary LND (17). In imaging studies, ultrasound is the most commonly used method for documenting and localizing lymph node recurrence due to the lack of radiation and high sensitivity and specificity (16). Stang et al. reported reoperations due to complications (hematoma) in patients who underwent transaxillary robotic thyroidectomy (18). In Kim’s retrospective study, 24 recurrent patients underwent robotic LND with or without completion thyroidectomy. However, the adhesions in lateral neck compartment and the extent of effect on reoperation were not described (19). In this study, we first reported a case of a patient that underwent completion thyroidectomy and LND after gasless transaxillary endoscopic thyroidectomy. The ultrasound test before the first treatment did not reveal abnormal lymph nodes in the central and lateral neck compartments. Further evaluation of the neck lymph nodes was not performed. Meanwhile, this patient did not participate in the originally planned follow-up at the 3- and 6-month visits. At the one-year visit, imaging tests revealed enlarged and suspicious malignant lymph nodes in levels III and IV of the lateral neck compartments. We believed that reoperation was performed for persistent, rather than truly recurrent, disease for this patient. During the second surgical procedure, we found that the surface of the IJV was significantly adhered to the surrounding fibroadipose tissue. The IJV was carefully dissected, revealing that the adhesions were only involved in the segments of the IJV located in level III. The adhesions of the IJV and omohyoid muscle did not affect the dissection of level II&IV Lymph nodes and affected only the dissection of the medial margin of level III lymph nodes. As long as the IJV is carefully dissected, possible IJV damage can be avoided, and the dissection of the lateral neck compartment can be performed successfully.
Conclusions
In conclusion, exposure of the lateral neck compartment in the gasless transaxillary procedure, especially exposure of the IJV, causes adhesions of the lateral neck compartment and brings difficulties for possible future LND. The IJV should be carefully dissected to avoid IJV injury, and the lateral neck compartment should be dissected successfully during reoperation. Gasless transaxillary endoscopic thyroid surgery should be performed in strictly selected patients with adequate preoperative assessment (5).
Acknowledgments
Funding: This work was funded by the National Natural Science Foundation of China (No. 82073262), Natural Science Foundation of Hunan province (Nos. 2019JJ4047 and 2021JJ41033) and China Postdoctoral Science Foundation (No. 2021M703641).
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at https://gs.amegroups.com/article/view/10.21037/gs-22-299/rc
Peer Review File: Available at https://gs.amegroups.com/article/view/10.21037/gs-22-299/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://gs.amegroups.com/article/view/10.21037/gs-22-299/coif). XL serves as an unpaid Honorary Editor-in-Chief of Gland Surgery from October 2022 to September 2023. The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. This study was approved by the institutional review board of Xiangya Hospital, Central South University (No. 202011960). All procedures performed in this study were in accordance with the Declaration of Helsinki (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Rossi L, Materazzi G, Bakkar S, et al. Recent Trends in Surgical Approach to Thyroid Cancer. Front Endocrinol (Lausanne) 2021;12:699805. [Crossref] [PubMed]
- Zhang Z, Sun B, Ouyang H, et al. Endoscopic Lateral Neck Dissection: A New Frontier in Endoscopic Thyroid Surgery. Front Endocrinol (Lausanne) 2021;12:796984. [Crossref] [PubMed]
- Piccoli M, Mullineris B, Gozzo D, et al. Evolution Strategies in Transaxillary Robotic Thyroidectomy: Considerations on the First 449 Cases Performed. J Laparoendosc Adv Surg Tech A 2019;29:433-40. [Crossref] [PubMed]
- Cong R, Li X, Ouyang H, et al. Gasless, endoscopic trans-axillary thyroid surgery: our series of the first 51 human cases. World J Surg Oncol 2022;20:9. [Crossref] [PubMed]
- Sun B, Li P, Cong R, et al. Gasless endoscopic transaxillary thyroid surgery: CUSUM analysis of a single surgeon's experience from 105 preliminary procedures. Surg Endosc 2022;36:8270-9. [Crossref] [PubMed]
- Russell JO, Sahli ZT, Shaear M, et al. Transoral thyroid and parathyroid surgery via the vestibular approach-a 2020 update. Gland Surg 2020;9:409-16. [Crossref] [PubMed]
- Sephton BM. Extracervical Approaches to Thyroid Surgery: Evolution and Review. Minim Invasive Surg 2019;2019:5961690. [Crossref] [PubMed]
- Jiang WJ, Yan PJ, Zhao CL, et al. Comparison of total endoscopic thyroidectomy with conventional open thyroidectomy for treatment of papillary thyroid cancer: a systematic review and meta-analysis. Surg Endosc 2020;34:1891-903. [Crossref] [PubMed]
- Berber E, Bernet V, Fahey TJ 3rd, et al. American Thyroid Association Statement on Remote-Access Thyroid Surgery. Thyroid 2016;26:331-7. [Crossref] [PubMed]
- Ouyang H, Xia F, Zhang Z, et al. Preoperative application of carbon nanoparticles in bilateral axillo-breast approach robotic thyroidectomy for papillary thyroid cancer. Gland Surg 2021;10:3188-99. [Crossref] [PubMed]
- He J, Zhang C, Zhang Z, et al. Evaluation of the clinical value of carbon nanoparticles in endoscopic thyroidectomy and prophylactic central neck dissection through total mammary areolas approach for thyroid cancer. World J Surg Oncol 2021;19:320. [Crossref] [PubMed]
- Wang D, Wang Y, Zhou S, et al. Transoral thyroidectomy vestibular approach versus non-transoral endoscopic thyroidectomy: a comprehensive systematic review and meta-analysis. Surg Endosc 2022;36:1739-49. [Crossref] [PubMed]
- Peng X, Li Z, Li H, et al. The clinical application of mental nerve dissection in transoral endoscopic thyroidectomy via an oral vestibular approach. Surg Endosc 2020;34:153-8. [Crossref] [PubMed]
- Bakkar S, Frustaci G, Papini P, et al. Track Recurrence After Robotic Transaxillary Thyroidectomy: A Case Report Highlighting the Importance of Controlled Surgical Indications and Addressing Unprecedented Complications. Thyroid 2016;26:559-61. [Crossref] [PubMed]
- Yan HC, Xiang C, Wang Y, et al. Scarless endoscopic thyroidectomy (SET) lateral neck dissection for papillary thyroid carcinoma through breast approach: 10 years of experience. Surg Endosc 2021;35:3540-6. [Crossref] [PubMed]
- Rivera-Robledo CG, Velázquez-Fernández D, Pantoja JP, et al. Recurrent Papillary Thyroid Carcinoma to the Cervical Lymph Nodes: Outcomes of Compartment-Oriented Lymph Node Resection. World J Surg 2019;43:2842-9. [Crossref] [PubMed]
- Raffaelli M, De Crea C, Sessa L, et al. Risk factors for local recurrence following lateral neck dissection for papillary thyroid carcinoma. Endocrine 2019;63:310-5. [Crossref] [PubMed]
- Stang MT, Yip L, Wharry L, et al. Gasless Transaxillary Endoscopic Thyroidectomy with Robotic Assistance: A High-Volume Experience in North America. Thyroid 2018;28:1655-61. [Crossref] [PubMed]
- Kim JK, Lee CR, Kang SW, et al. Robotic transaxillary lateral neck dissection for thyroid cancer: learning experience from 500 cases. Surg Endosc 2022;36:2436-44. [Crossref] [PubMed]


