
Comparison between pancreatic duct guide wire-assisted needle knife precut and conventional needle knife precut for periampullary diverticula with difficult cannulation: a retrospective comparative cohort study
IntroductionOther Section
Periampullary diverticula (PAD) is a common disease of the digestive tract, and its incidence increases with age. The detection rate of PAD in endoscopic retrograde cholangiopancreatography (ERCP) is 5–27%, with an average of approximately 17% (1). PAD is more frequently diagnosed due to the wide application of ERCP. A previous study has reported on the relationship between PAD and bile duct stones, and the incidence of bile duct stones in PAD patients is significantly increased (2). ERCP remains the primary approach to treating bile duct stones, and papilla cannulation plays a critical role in the success of ERCP. The diverticulum often oppresses the pancreatic and bile duct, leading to changes in their directions. Meanwhile, the papilla is vulnerable to the chemical stimulation of food residues and induces bacterial infection, resulting in diverticulitis and papillitis. These factors often increase the difficulty of cannulation (3-5), leading to frequent cannulation failure in the presence of PAD (6).
Special ancillary cannulation methods, such as the precut through the pancreatic duct, guide wire-assisted or stent-assisted pancreatic duct precut, do not had very high cannulation success rates, especially in cases with PAD (7). The precut of the papilla was first proposed in 1980, and the subsequent needle knife precut greatly promoted the clinical application of precut incision (8). The precut can be performed by the needle knife directly. Sometime the pancreatic duct guide wire or stent can be used to aid the needle knife; However, this approach also increases the risk of various adverse events, such as bleeding, perforation, pancreatitis, and cholangitis (9,10), especially in cases with PAD. Therefore, it is critically necessary to develop an effective way of improving the cannulation success rate in patients with PAD.
In the present study, we aimed to compare pancreatic duct guide wire-assisted needle knife precut (Group A) and conventional needle knife precut (Group B) in PAD patients with difficult cannulation. Moreover, the clinical outcomes were analyzed to assess any differences in the cannulation success rates, complications, and operating time between the two groups. We present the following article in accordance with the STROBE reporting checklist (available at https://gs.amegroups.com/article/view/10.21037/gs-22-524/rc).
MethodsOther Section
A total of 230 cases of PAD with difficult cannulation of the duodenal papilla diagnosed by ERCP between June 2009 and December 2021 were retrospectively reviewed. The exclusion criteria were set as follows: patients with ERCP history, coagulopathy [prothrombin time two times longer or platelet (PLT) count ≤70×109], or an inability to tolerate endoscopy due to severe heart/lung diseases. Among the 230 included cases, pancreatic duct guide wire-assisted needle knife precut (Group A) was performed in 135 cases, and conventional needle knife precut (Group B) was performed in 95 cases. There were no differences in age and sex between the two groups, also no statistical difference in disease distribution between the two groups (Table 1). All procedures were performed using side-viewing endoscopes (TJF-260; Olympus Optical Corporation, Tokyo, Japan). ERCP was performed by experienced endoscopists at a single center. Cannulation was attempted using an ERCP catheter or a pull-type sphincterotomy.
Table 1
| Clinical variables | Group A (n=135) | Group B (n=95) | P value |
|---|---|---|---|
| Age (mean ± standard deviation) | 66.89±15.85 | 61.32±18.70 | 0.28 |
| Sex (female/male) | 45/90 | 35/60 | 0.656 |
| Bile duct stones | 79 | 56 | 1 |
| Bile duct or pancreatic tumor | 41 | 30 | 0.885 |
| Cholangitis strictures | 15 | 9 | 0.698 |
Before the operation, 10 mg of anisodamine was intravenously injected to inhibit intestinal peristalsis and glandular secretion. In addition, 50 mg of pethidine and 10 mg of diazepam were intravenously injected for sedation and pain relief. The operating procedure was as follows. The endoscope entered the duodenum, and the papilla was located. When conventional cannulation failed and the guide wire was cannulated into the pancreatic duct, the guide wire was retained, and a precut technique using a needle knife was applied (Group A). The precut was performed on the left guide wire according to the biliary axis, and the operation was conducted layer-by-layer with caution. When a white choledochal sphincter was observed, the precut was stopped.
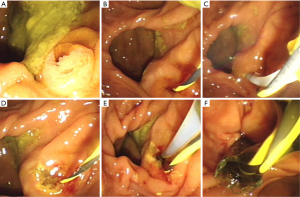
Intraoperatively, a clear vision was maintained. If bleeding occurred, norepinephrine saline was used to irrigate the wound. If the cannulation was not successful, the precut was performed again in the choledochal sphincter until successful cannulation was achieved. The pancreatic stent was implanted in the pancreatic duct along the guide wire after successful bile duct cannulation. A nasobiliary tube was implanted in the bile duct for 3–5 days (Figure 1). When conventional cannulation failed, the guide wire could not enter the biliopancreatic duct (Group B). We then used the needle knife to precut according to the biliary axis. The operation process in Group B was the same as that in Group A. If the precut was successful, a nasobiliary tube was implanted in the bile duct for 3–5 days.
All of the patients were asked about the presence and timing of certain symptoms, including abdominal pain, fever, and jaundice. The incidence and frequency of complications, such as bleeding, perforation, cholangitis, and pancreatitis, were compared between Groups A and B. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). This study was approved by the Ethics Committee of the First People’s Hospital of Changzhou [No. 23(2018)]. Informed consent was taken from all the patients.
Statistical analysis
SPSS20.0 statistical software (Developed by SPSS, Chicago, USA) was used for the t-test and analysis of variance. P<0.05 was considered statistically significant.
ResultsOther Section
Table 1 presents the demographic characteristics of the 230 patients (150 males and 80 females). The median operating time of the needle knife precut was significantly shorter in Group A, with a median time of 18.44±6.65 min, compared with 32.05±13.15 min in Group B. Also, the success rate of the cannulation was markedly higher in Group A (100%, 135/135) compared with Group B (78.9%, 75/95). The differences in the operating times and the cannulation success rates were significant.
Intraoperative complications mainly included bleeding (15/135) in Group A and bleeding (24/95) and perforation (2/95) in Group B, which occurred in 15 (11.1%) and 26 (27.4%) cases in Groups A and B, respectively. Postoperative complications mainly comprised post-ERCP pancreatitis, which occurred in 10 (7.4%) and 17 (17.9%) cases in Groups A and B, respectively. The differences in intraoperative and postoperative complication rates between the groups were significant (P<0.01). All cases of bleeding and pancreatitis were mild and treated conservatively. Cases involving perforation were clipped with titanium clips and recovered well after the operation (Table 2).
Table 2
| Variables | Group A | Group B | P value |
|---|---|---|---|
| No. of patients | 135 | 95 | |
| Operating time, min (mean ± standard deviation) | 18.44±6.65 | 32.05±13.15 | 0.001 |
| Intraoperative perforation | 0 | 2 | 0.331 |
| Intraoperative bleeding | 15 | 24 | 0.001 |
| Postoperative complications | 10 | 17 | 0.001 |
| Success rate of cannulation | 100% | 78.9% | 0.001 |
DiscussionOther Section
PAD is a common disease of the digestive tract. The previous study has divided it into three types: type I (internal diverticulum), type II (marginal diverticulum papilla), and type III (para diverticulum) (11). It can also be divided into two types: type I—external papilla of the diverticulum, and type II—internal papilla of the diverticulum. The diverticulum often oppresses the bile and pancreatic duct, causing them to change their directions. Meanwhile, the diverticulum is easily stimulated by food residues, which causes diverticulitis and papillitis, leading to increased difficulty in cannulation.
The needle knife precut is an effective method for difficult cannulation. However, it also has some risks, such as hemorrhage and perforation, especially to the diverticulum. For cases of PAD with difficult cannulation, pancreatic duct guide wire-assisted needle knife precut sphincterotomy has the following advantages. Firstly, PAD often changes the biliary axis, making it difficult to precut in an appropriate direction. A pancreatic duct guide wire can adjust the papilla to the ideal position, which is very useful to the precut. Secondly, some PAD papillae are distant from the duodenal lens, increasing the risk of precut and reducing the precut success rate. The guide wire of the pancreatic duct can adjust the papilla to the appropriate position, which is favorable for precut. Thirdly, cases of partial PAD often cause papilla to collapse. In such cases, conventional precut can not be performed at all, while the pancreatic duct wire can pull out the papilla from the diverticulum for the precut. Fourthly, in some PAD cases, the papilla is affected by respiration and its activity is very high. Direct precut is very difficult to grasp the depth, often resulting in perforation and other complications. Pancreatic duct wire plays a supporting role in the fixed papilla and increases the precut success rate.
In cases of PAD, when the needle knife is used to precut, attention should be paid to the following points. Firstly, judging the correct direction of the bile duct is critical, especially for cases with papilla deviation. It is not the normal location from 11 to 12 points. The left side of the pancreatic duct guide wire can be cut off according to the biliary axial. Secondly, the cut should be performed layer-by-layer. The shallow cut often causes papilla bleeding and precut failure. Meanwhile, the deep cut often causes perforation. Thirdly, it is particularly important to pay attention to the difference between the choledochal sphincter and the surrounding mucosa. In addition, the papilla is cut as much as possible to locate the choledochal sphincter.
In this study, the incidence of intraoperative and postoperative complications was higher in Group B compared with Group A. Also, bleeding was a common complication of needle knife precut in the two groups. All cases of bleeding were mild and were effectively controlled following electric coagulation or balloon compression. Previous studies have reported that perforation is the most serious complication of needle knife precut (12,13). Two cases occurred in Group B, which were promptly clipped with titanium clips, and the patients recovered well after the operation. In contrast, no perforation occurred in Group A. The main postoperative complication was pancreatitis, which was lower in Group A compared with Group B. The reason for this could be attributed to the long operating time in Group B, which could easily result in papillary edema and increase the incidence of pancreatitis. However, in Group A, the operating time was short, and most patients were implanted with pancreatic duct stents postoperatively. Previous studies have reported that pancreatic stent placement significantly reduces the incidence of postoperative pancreatitis (14,15).
In conclusion, pancreatic duct guide wire-assisted needle knife precut appeared to be a safe and effective modality for cases of PAD with difficult cannulation. It had a higher cannulation success rate and fewer operative complications. Nevertheless, considering that the present study was limited by its retrospective nature and a relatively small cohort, a large prospective study is needed to analyze the clinical feasibility of performing pancreatic duct guide wire-assisted needle knife precut in cases with PAD.
AcknowledgmentsOther Section
Funding: This research was funded by the Changzhou Applied Basic Research Program (No. CJ20210074). The funders had no role in the study design, data collection and analysis, decision to publish, or preparation of the manuscript.
FootnoteOther Section
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at https://gs.amegroups.com/article/view/10.21037/gs-22-524/rc
Data Sharing Statement: Available at https://gs.amegroups.com/article/view/10.21037/gs-22-524/dss
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://gs.amegroups.com/article/view/10.21037/gs-22-524/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). This study was approved by the Ethics Committee of the First People’s Hospital of Changzhou [No. 23(2018)]. Informed consent was taken from all the patients.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
ReferencesOther Section
- Sun Z, Bo W, Jiang P, et al. Different Types of Periampullary Duodenal Diverticula Are Associated with Occurrence and Recurrence of Bile Duct Stones: A Case-Control Study from a Chinese Center. Gastroenterol Res Pract 2016;2016:9381759. [Crossref] [PubMed]
- Alzerwi NAN. Recurrent ascending cholangitis with acute pancreatitis and pancreatic atrophy caused by a juxtapapillary duodenal diverticulum: A case report and literature review. Medicine (Baltimore) 2020;99:e21111. [Crossref] [PubMed]
- Kuo CM, Chiu YC, Liang CM, et al. Limited precut sphincterotomy combined with endoscopic papillary balloon dilation for common bile duct stone removal in patients with difficult biliary cannulation. BMC Gastroenterol 2016;16:70. [Crossref] [PubMed]
- Tomishima K, Ishii S, Fujisawa T, et al. Does restricting fluid volume impact post-ERCP pancreatitis in patient with heart disease? Saudi J Gastroenterol 2021;27:355-60. [Crossref] [PubMed]
- Cennamo V, Fuccio L, Zagari RM, et al. Can early precut implementation reduce endoscopic retrograde cholangiopancreatography-related complication risk? Meta-analysis of randomized controlled trials. Endoscopy 2010;42:381-8. [Crossref] [PubMed]
- Jayaraj M, Mohan BP, Dhindsa BS, et al. Periampullary Diverticula and ERCP Outcomes: A Systematic Review and Meta-Analysis. Dig Dis Sci 2019;64:1364-76. [Crossref] [PubMed]
- Klair JS, Nakshabendi R, Rajput M, et al. Pancreatic Mass or Cyst? Diagnostic Dilemma. Dig Dis 2019;37:521-4. [Crossref] [PubMed]
- Kalayci MU, Altintas T. Can Early 'Shallow' Needle-knife Papillotomy be the First Choice in ERCP? Surg Laparosc Endosc Percutan Tech 2020;30:180-2. [Crossref] [PubMed]
- Sasahira N, Kawakami H, Isayama H, et al. Early use of double-guidewire technique to facilitate selective bile duct cannulation: the multicenter randomized controlled EDUCATION trial. Endoscopy 2015;47:421-9. [Crossref] [PubMed]
- Tse F, Liu J, Yuan Y, et al. Guidewire-assisted cannulation of the common bile duct for the prevention of post-endoscopic retrograde cholangiopancreatography (ERCP) pancreatitis. Cochrane Database Syst Rev 2022;3:CD009662. [PubMed]
- Chandy G, Hart WJ, Roberts-Thomson IC. An analysis of the relationship between bile duct stones and periampullary duodenal diverticula. J Gastroenterol Hepatol 1997;12:29-33. [Crossref] [PubMed]
- Zhou PH, Yao LQ, Xu MD, et al. Application of needle-knife in difficult biliary cannulation for endoscopic retrograde cholangiopancreatography. Hepatobiliary Pancreat Dis Int 2006;5:590-4. [PubMed]
- Furuya CK, Sakai P, Marinho FRT, et al. Papillary fistulotomy vs conventional cannulation for endoscopic biliary access: A prospective randomized trial. World J Gastroenterol 2018;24:1803-11. [Crossref] [PubMed]
- Shin SH, So H, Cho S, et al. The number of wire placement in the pancreatic duct and metal biliary stent as risk factors for post-endoscopic retrograde cholangiopancreatography pancreatitis. J Gastroenterol Hepatol 2020;35:1201-7. [Crossref] [PubMed]
- Sakr C, Harb M, Makhoul E. The role of double-guidewire technique in preventing postendoscopic retrograde cholangiopancreatography pancreatitis. Arab J Gastroenterol 2021;22:133-6. [Crossref] [PubMed]
(English Language Editor: A. Kassem)



