
A case series study of lacrimal canalicular laceration repair with the bi-canalicular stent
Introduction
Lacrimal canalicular laceration can be caused by trauma on the ocular adnexa, such as penetrating or blunt injuries, accounting for approximately 16% of eyelid lacerations and 20% of eye traumas (1,2).
Traumatic canalicular laceration is commonly considered an ophthalmologic emergency. Ejstrup et al. reported that 72% of lower canaliculus lacerations are mono-canalicular, and bi-canalicular lacerations account for 6% to 24% of all canalicular injuries (3,4). Symptomatic epiphora can be caused by wounds that are not precisely repaired, especially in patients with lacerations to their lower canaliculus. Therefore, emergency surgery can reduce the risk of missing the severed ends of the lacrimal system, which typically requires surgery within 48 hours of the trauma (4).
Based on the mechanisms of damage, lacrimal canalicular lacerations can be divided into direct (e.g., knife and dog bite), indirect (e.g., blunt force and blow), and diffuse injuries (e.g., orbital fracture, globe rupture).
The treatment of traumatic canalicular laceration varies widely, and different surgical techniques have been described by different authors. Medical-grade silicone has been a preferred material for stenting torn canaliculi clinically, such as the Freda® silicone tube, mini-Monoka®, and Masterka® tube. Historically, canalicular anastomosis combined with bi-canalicular or mono-canalicular stent intubation has been used for canalicular laceration repair. Bi-canalicular intubation has been found to have high rates of successful repair (5,6). Moreover, bi-canalicular stents can provide appropriate tension of lacerated ends, making it a more effective approach of medial canthal tendon repair (7,8).
Henan province is the largest agricultural province in central China, which is the biggest developing country. This study was a retrospective study of 338 patients with traumatic lacrimal canalicular lacerations in Henan Provincial People’s Hospital, China. We described the epidemiology and evaluated the clinical outcomes of reparation using a bi-canalicular stent in central China, provide reference for clinical work. We present the following article in accordance with the STROBE reporting checklist (available at https://gs.amegroups.com/article/view/10.21037/gs-22-556/rc).
Methods
This study is a comprehensive review of 338 patients (338 eyes) with eyelid lacrimal canaliculus lacerations undergoing reparative bi-canalicular stent intubation in Henan Eye Hospital, Henan Provincial People’s Hospital between 2017 and 2020. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by ethics committee of Henan Eye Institute, Henan Eye Hospital, Henan Provincial People’s Hospital (No. HNEEC-2022-37-01) and informed consent was taken from all the patients and patients’ guardians.
The analyzed data included demographics, the environment of the trauma, mechanisms of injury, additional injury, and surgical outcomes at follow-up. The outcomes included anatomic success, functional success, and complications. Diagnostic exploration of lacrimal duct patency was defined as anatomical success. Moreover, a canaliculus without epiphora after stent removal was defined as functional success. The exclusion criteria included lack of adequate follow-up (<3 months), tear spillage and pus prior to injury, including the lacrimal sac and/or nasolacrimal duct, and severe life-threatening trauma.
All patients were examined under general anesthesia and underwent adequate debridement. The canalicular laceration’s proximal end was located through the operating microscope. Then, the punctum was appropriately enlarged using a lacrimal punctum dilator. A lacrimal probe with a rigid guidewire was inserted through the punctum into the ruptured tubule and nasal cavity, and the rigid guidewire was pulled out from the nasal cavity. Then, the silicone tube was pulled out of the punctum from the nasal cavity. In the same way, a 5-0 prolene suture was pulled out of the other canalicular punctum. Next, the prolene suture guided the tube throughout the other canaliculus from the nasal cavity. Finally, the 2 ends of the silicone tube at a proper length were securely tied in the nasal cavity with a 6-0 absorbable suture made of polydioxanone (Johnson & Johnson, USA). The lacerated ends were meticulously anastomosed with 6-0 absorbable polydioxanone sutures around the silicone tube under an ophthalmic surgical microscope (Figure 1). Globe wound repair was performed by experienced surgeons when a globe injury occurred.
Statistical analysis
The statistics, including the mean, standard deviation, and range, were calculated for different variables. Statistical analysis was performed using SPSS software (version 19.0, IBM, USA). Continuous data were expressed as mean ± standard deviation. Continuous variables were analyzed by Student’s t-test, and categorical variables were analyzed by the χ2 test or Fisher’s exact test. P value <0.05 was considered significant.
Results
Among the 338 patients, 254 (75.15%) patients were males and 84 (24.85%) patients were females. The mean age was 39.6±20.0 years of age (1 to 88 years). Upper and lower canalicular lacerations were seen in 68 (20.12%) and 256 patients (75.74%), respectively, while both canalicular lacerations were seen in 14 patients (4.14%; Table 1).
Table 1
| Parameters | Patient numbers |
|---|---|
| Total patients | 338 |
| Age (years) | 39.6±20.0 (1 to 88) |
| Males | 254 (75.15) |
| Females | 84 (24.85) |
| Eye involved | |
| Right | 161 (47.63) |
| Left | 177 (52.37) |
| Canalicular involved | |
| Upper | 68 (20.12) |
| Lower | 256 (75.74) |
| Both | 14 (4.14) |
| Environment of injury | |
| Family home | 111 (32.84) |
| Construction site | 36 (10.65) |
| Public building and place | 22 (6.51) |
| Street and road | 146 (43.20) |
| Agricultural environment | 23 (6.80) |
| Type of trauma | |
| Sharp object | 64 (18.93) |
| Dog bite | 7 (2.07) |
| Explosion injury | 8 (2.37) |
| Blunt injury | 42 (12.43) |
| Traffic accident/electric bike accident | 127 (37.57)/72 (21.30) |
| Fall | 65 (19.23) |
| Fight | 25 (7.40) |
| Additional injury | |
| Globe rupture | 34 (10.06) |
| Optic neuropathy | 5 (1.48) |
| Tarsus laceration | 115 (34.02) |
| Head trauma | 2 (0.59) |
| Orbital wall fracture | 41 (12.13) |
| Periocular or intraocular foreign body | 10 (2.96) |
Data are presented as mean ± standard deviation (range) or n (%).
In regards to the place of injury occurrence, streets ranked first (146 patients, 43.20%), followed by home (111 patients, 32.84%), construction site (36 patients, 10.65%), agricultural workplace (23 patients, 6.80%), and public areas (22 patients, 6.51%).
Table 1 shows the causes of injury. Traffic accidents were the leading cause of injury, including 72 (21.30%) cases of electric bike-associated accidents, followed by fall-related trauma in 65 (19.23%) patients, sharp object injury in 64 (18.93%) patients, blunt injury in 42 (12.43%) patients, fight-related trauma in 25 (7.40%) patients, dog bites in 7 (2.07%) patients, and explosion-related injury in 8 (2.37%) patients (Table 1).
Additional injuries associated with lacrimal canalicular laceration are shown in Table 1. A total of 207 (61.24%) patients had additional injuries: 41 (12.13%) patients had orbital wall fractures, 34 (10.06%) patients had globe rupture, 10 (2.96%) patients had periocular or intraocular foreign bodies, 5 (1.48%) patients had optic neuropathies, and 2 (0.59%) patients had head trauma.
The mean time of bi-canalicular stent removal was 3.2±0.97 months (from 3 to 6 months). Concerning the surgery complications in our study, there were 0 (0%) patients with false path, 6 (1.78%) patients with eyelid ectropion, and 9 (2.66%) patients with stent extrusion and loss due to eye rubbing and pulling the sutures out. During the following-up visits, no patient developed lacrimal canaliculus duct infection.
We defined anatomic success as gently use a lacrimal probe to diagnostically access the lacrimal sac and functional success as the lack of postoperative epiphora. Among the 324 (95.86%) patients who demonstrated anatomic success and had excellent cosmetic results, 303 (89.64%) patients had functional success (Table 2).
Table 2
| Canaliculus involved | Anatomic success, n (%) | Functional success, n (%) |
|---|---|---|
| Upper | 66 (97.06) | 60 (91.18) |
| Lower | 245 (95.70) | 232 (90.63) |
| Both | 13 (92.86) | 11 (85.71) |
Discussion
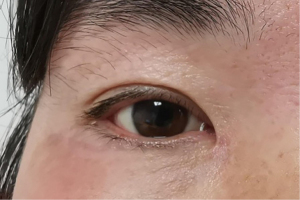
The lacrimal portion of the eyelid is a physiologically and anatomically specialized drainage zone and is the weakest portion for indirect canalicular lacerations secondary to blunt tangential eyelid or cheek blows. The mechanism of canalicular laceration was described in detail by Jordan et al. (9). The medial lacrimal portion of the eyelid, containing the canaliculus and Horner’s muscle, is devoid of tarsus and lacks surrounding connective tissue. Furthermore, they concluded that the superomedial bony orbital rim and side of the nose act as a funnel with the canalicular system lying at its base. This funnel directionally facilitates any approaching slender object in providing access to the canalicular region of the eyelid (10). Sequelae such as ectropion, epiphora, and poor cosmetic result can occur if the canalicular laceration is not properly managed in time (Figure 2).

Although there have been some reports on the epidemiology of canalicular laceration, the type and location of trauma that causes these injuries has changed due to changes in people’s lifestyles and regional differences.
In our study, 3/4 of cases were males (75.15%). Upper and lower canalicular lacerations were seen in 68 patients (20.12%) and 256 patients (75.74%), respectively, while both canalicular lacerations were seen in 14 patients (4.14%). The age was similar to previous studies (11-13). Kennedy et al. noted that 68% of patients were younger than 30 years of age (11). Research published by Naik et al. in 2008 reported that the mean age of patients was 16 years old in India (8). In 2017, Alam et al. found a similar mean age of patients of 19.3 years of age (1).
However, the mean age of patients with canalicular lacerations was 39.6 years of age in this study, which was similar to the reports of Lin et al. in Taiwan in 2019 (12) as well as Guo et al. in Shanghai in 2020 (13). The large difference in mean age might be due to the variation in injury mechanism and place of occurrence in different countries.
In our study, the most common place of trauma occurrence was the streets (43.20%). The corresponding type of injury was traffic accidents (37.57%), the most common being electric bike accidents, accounting for 72 cases (21.30%), which was similar to that of other study (14).
The home was the second most frequent place of injury occurrence (32.84%), followed by construction sites (10.65%) and agricultural workplaces (6.80%). This assessment reveals important information that warrants discussion. In central China, agricultural industrialization reform has had remarkable results. A large population lives in the rural area of Henan province. Moreover, many people use their residential property for commercial purposes, having workshops at their homes.
The second most frequent cause of canaliculus laceration was fall-related trauma (19.23%), followed by sharp object injury (18.93%), blunt injury (12.43%), fight-related trauma (7.40%), dog bite (2.07%), and explosion-related injury (2.37%). All patients who experienced dog bites were children in rural areas. Our data showed that indirect canalicular injuries were significantly more predominant than direct injury, which was also shown by Wulc et al. (15).
Our study showed that there were 115 (34.02%) patients with tarsus lacerations. This rate was similar to the results derived by Guo et al. (13). Canalicular lacerations combined with globe rupture occurred in 34 (10.06%) patients. The other additional injuries were as follows: 41 (12.13%) orbital wall fractures, 10 (2.96%) periocular or intraocular foreign bodies, 2 (0.59%) head trauma, and 5 (1.48%) optic neuropathies. There is no previous information available on the incidence of open globe injury and orbital wall fractures during canalicular laceration. Lee et al. reported that traumatic subconjunctival hemorrhage was the most common associated ocular injury (16). Herzum et al. reported that there was a 20% to 44% incidence rate for globe injury in association with eyelid injuries (2). In our series, the epidemiology was different from theirs.
There are a few key factors that affect the effectiveness of laceration repair, including the extent and location of canalicular lacerations, the intubation materials, the duration of intubation, and the surgical technique (17-19).
According to our clinical experience, it is believed that a successful canaliculus repair operation requires 3 key steps. The first step is to find the proximal lacerated end quickly and accurately. The second step is the canalicular silicone stent intubation without iatrogenic injury to an intact canaliculus. The last step is meticulous canalicular anastomosis around the silicone stent to provide patency for the lacrimal drainage system and closure of the surrounding eyelid soft tissue.
Locating the proximal lacerated end of the canaliculus requires understanding of the medial canthal anatomy, as described by Jordon et al. (9). There are many assisted methods for locating the end. Pigtail probing or injecting air, fluorescein dye, or viscoelastic substances from one punctum to identify the other end have been reported (20-22). Peng et al. described a method to identify torn ends of the canaliculus using a 23 Ga fiber optic probe (23).
In our study, all the proximal ends of the canalicular lacerations were successfully and intuitively located through a surgical microscope without any assistance. However, this may not be effective under all circumstances. We believe that the method described above may prove to be a salvage technique if the medial canalicular lacerated end is not identified after a period of time of careful searching.
Medical-grade silicone intubation is commonly used in surgery for canalicular laceration repair because of its advantages, such as its inert property, pliability, and availability (24). In the early stages of canalicular laceration, severe eyelid edema and persistent bleeding can occur during the operation. Hence, the placement of the stent can be challenging in canalicular repairs. Moreover, the surgeon should carefully use the lacrimal punctum dilator and lacrimal probe as far as possible to reduce the risk of damaging the canalicular system and creating a false passage. In our study, there was no patient with false paths.
Bi-canalicular stents typically create a closed-loop system which decreases the likelihood of extrusion. Tint et al. reported that the Crawford stent allows medial and posterior traction on the canalicular system, thereby aiding the adequate repositioning of the eyelid and counteracting the inferolateral tension exerted by the orbicularis muscle (25).
In our study, all of the patients were operated on by professional surgeons with the meticulous technique of peri-canalicular repair combined with stent intubation, rather than direct canalicular wall suture, which can further damage the delicate mucosa and induce a suture reaction and tearing of the canalicular wall.
Although there is no consensus regarding the exact duration of a canalicular stent to achieve long-term canalicular patency, most surgeons propose a longer duration (8,26,27). In this study, bi-canalicular stents were maintained for 3.2 months. The stents were in place for 3 to 6 months, and the canaliculus healed and formed an epithelialized channel around the stent when the stent was removed (21).
We defined anatomic success as softly diagnostic probing to sac and functional success as the lack of postoperative epiphora. In our series, there were 6 (1.78%) patients with eyelid ectropion and 9 (2.66%) patients with stent extrusion and/or loss because the patients had rubbed their eyes and pulled the suture out. Some previous studies showed that urgent canalicular lacerations had an anatomic success rate of 25–94.1%, a functional success rate of 58–100% (8,26,28,29), and an extrusion rate of 5.88–23.2% (8,16,30-32). Our study had a higher anatomic success rate (95.86%), similar functional success rate (89.64%), and low postoperative complication rate (4.45%).
The primary important reason for anatomic failure and functional failure might be lacrimal drainage system blockage, such as canalicular stenosis, peri-canalicular scarring band, or malposition of the punctum due to injury of the Horner muscle and orbicularis oculi (19).
In conclusion, electric bike accidents occurring on the streets and fall-related lacrimal trauma are the top 2 leading causes of injury nowadays because of the location-dependent lifestyle of people living in Henan province.
Though our study was retrospective and non-comparative in nature, a larger scale, comparative study with a longer period of observation is necessary in the future. The laceration repair with a bi-canalicular stent evaluated in this study provides an effective surgical therapeutic strategy for lacrimal canalicular laceration.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at https://gs.amegroups.com/article/view/10.21037/gs-22-556/rc
Data Sharing Statement: Available at https://gs.amegroups.com/article/view/10.21037/gs-22-556/dss
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://gs.amegroups.com/article/view/10.21037/gs-22-556/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by ethics committee of Henan Eye Institute, Henan Eye Hospital, Henan Provincial People’s Hospital (No. HNEEC-2022-37-01) and informed consent was taken from all the patients and patients’ guardians.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Alam MS, Mehta NS, Mukherjee B. Anatomical and functional outcomes of canalicular laceration repair with self retaining mini-MONOKA stent. Saudi J Ophthalmol 2017;31:135-9. [Crossref] [PubMed]
- Herzum H, Holle P, Hintschich C. Eyelid injuries: epidemiological aspects. Ophthalmologe 2001;98:1079-82. [Crossref] [PubMed]
- Ejstrup R, Wiencke AK, Toft PB. Outcome after repair of concurrent upper and lower canalicular lacerations. Orbit 2014;33:169-72. [Crossref] [PubMed]
- Ducasse A, Arndt C, Brugniart C, et al. Lacrimal traumatology. J Fr Ophtalmol 2016;39:213-8. [Crossref] [PubMed]
- Mansour HO, Ramadan Ezzeldin E. Bicanalicular Annular Stent Compared with Bicanalicular Nasal Intubation in Management of Traumatic Lower Canalicular Laceration. Clin Ophthalmol 2022;16:213-22. [Crossref] [PubMed]
- Yan CF. Efficacy of double lacrimal duct placement with mitomycin in the treatment of recurrent tear duct membrane closure. Journal of Practical Medical Techniques 2021;28:80-1.
- Cho SH, Hyun DW, Kang HJ, et al. A simple new method for identifying the proximal cut end in lower canalicular laceration. Korean J Ophthalmol 2008;22:73-6. [Crossref] [PubMed]
- Naik MN, Kelapure A, Rath S, et al. Management of canalicular lacerations: epidemiological aspects and experience with Mini-Monoka monocanalicular stent. Am J Ophthalmol 2008;145:375-80. [Crossref] [PubMed]
- Jordan DR, Ziai S, Gilberg SM, et al. Pathogenesis of canalicular lacerations. Ophthalmic Plast Reconstr Surg 2008;24:394-8. [Crossref] [PubMed]
- Kim T, Yeo CH, Chung KJ, et al. Repair of Lower Canalicular Laceration Using the Mini-Monoka Stent: Primary and Revisional Repairs. J Craniofac Surg 2018;29:949-52. [Crossref] [PubMed]
- Kennedy RH, May J, Dailey J, et al. Canalicular laceration. An 11-year epidemiologic and clinical study. Ophthalmic Plast Reconstr Surg 1990;6:46-53. [Crossref] [PubMed]
- Lin CH, Wang CY, Shen YC, et al. Clinical Characteristics, Intraoperative Findings, and Surgical Outcomes of Canalicular Laceration Repair with Monocanalicular Stent in Asia. J Ophthalmol 2019;2019:5872485. [Crossref] [PubMed]
- Guo T, Qin X, Wang H, et al. Eiology and prognosis of canalicular laceration repair using canalicular anastomosis combined with bicanalicular stent intubation. BMC Ophthalmol 2020;20:246. [Crossref] [PubMed]
- Bai F, Tao H, Zhang Y, et al. Old canalicular laceration repair: a retrospective study of the curative effects and prognostic factors. Int J Ophthalmol 2017;10:902-7. [PubMed]
- Wulc AE, Arterberry JF. The pathogenesis of canalicular laceration. Ophthalmology 1991;98:1243-9. [Crossref] [PubMed]
- Lee H, Chi M, Park M, et al. Effectiveness of canalicular laceration repair using monocanalicular intubation with Monoka tubes. Acta Ophthalmol 2009;87:793-6. [Crossref] [PubMed]
- Chu YC, Wu SY, Tsai YJ, et al. Early Versus Late Canalicular Laceration Repair Outcomes. Am J Ophthalmol 2017;182:155-9. [Crossref] [PubMed]
- Singh S, Ganguly A, Hardas A, et al. Canalicular lacerations: Factors predicting outcome at a tertiary eye care centre. Orbit 2017;36:13-8. [Crossref] [PubMed]
- Singh M, Gautam N, Ahir N, et al. Is the distance from punctum a factor in the anatomical and functional success of canalicular laceration repairs? Indian J Ophthalmol 2017;65:1114-9. [Crossref] [PubMed]
- Örge FH, Dar SA. Canalicular laceration repair using a viscoelastic injection to locate and dilate the proximal torn edge. J AAPOS 2015;19:217-9. [Crossref] [PubMed]
- Kwitny A, Baker JD. Functional results of the surgical repair of a lacerated canaliculus in children. J Pediatr Ophthalmol Strabismus 2011;48:117-9. [Crossref] [PubMed]
- Liu B, Li Y, Long C, et al. Novel air-injection technique to locate the medial cut end of lacerated canaliculus. Br J Ophthalmol 2013;97:1508-9. [Crossref] [PubMed]
- Peng W, Wang Y, Tan B, et al. A new method for identifying the cut ends in canalicular laceration. Sci Rep 2017;7:43325. [Crossref] [PubMed]
- Reifler DM. Management of canalicular laceration. Surv Ophthalmol 1991;36:113-32. [Crossref] [PubMed]
- Tint NL, Alexander P, Cook AE, et al. Eyelid avulsion repair with bi-canalicular silicone stenting without medial canthal tendon reconstruction. Br J Ophthalmol 2011;95:1389-92. [Crossref] [PubMed]
- Murchison AP, Bilyk JR. Canalicular laceration repair: an analysis of variables affecting success. Ophthalmic Plast Reconstr Surg 2014;30:410-4. [Crossref] [PubMed]
- Drnovsek-Olup B, Beltram M. Trauma of the lacrimal drainage system: retrospective study of 32 patients. Croat Med J 2004;45:292-4. [PubMed]
- Leibovitch I, Kakizaki H, Prabhakaran V, et al. Canalicular lacerations: repair with the Mini-Monoka® monocanalicular intubation stent. Ophthalmic Surg Lasers Imaging 2010;41:472-7. [Crossref] [PubMed]
- Rosser PM, Burt B, Osborne SF. Determination of the function of a repaired canaliculus after monocanalicular injury by placing a punctal plug in the non-involved punctum on the affected side. Clin Exp Ophthalmol 2010;38:786-9. [Crossref] [PubMed]
- Chowdhury HR, Rose GE, Ezra DG. Long-term outcomes of monocanalicular repair of canalicular lacerations. Ophthalmology 2014;121:1665-6.e1. [Crossref] [PubMed]
- Eo S, Park J, Cho S, et al. Microsurgical reconstruction for canalicular laceration using Monostent and Mini-Monoka. Ann Plast Surg 2010;64:421-7. [Crossref] [PubMed]
- Raj A, Thakur S, Arya KS, et al. Canalicular lacerations in a tertiary eye hospital: our experience with monocanalicular stents. Rom J Ophthalmol 2020;64:146-52. [Crossref] [PubMed]
(English Language Editor: C. Betlazar-Maseh)


