
Comparison of [18F]fluorocholine PET/CT with [99mTc]sestamibi and ultrasonography to detect parathyroid lesions in primary hyperparathyroidism: a prospective study
Introduction
Primary hyperparathyroidism (pHPT) is a common endocrine disorder produced by a disproportionate increase of parathyroid hormone (PTH) due to a benign adenoma of a single parathyroid gland (80–85% of cases) or as multiple gland hyperplasia (5–15% of cases) or as a rare malignant tumor (0.5–5% of cases) (1,2). Parathyroidectomy is the only curative treatment of pHPT but the surgical techniques have evolved considerably during the last decades. Bilateral neck exploration and surgery to resect enlarged parathyroid glands have been the gold standard procedures for patients with pHPT (3), although in cases of variable number or ectopic locations of parathyroid glands, intraoperative identification based on visual inspection and palpation can be difficult causing failure of surgery with persistent hypoparathyroidism (4). However, given that a single parathyroid adenoma is the cause of the disease in more than 80% of patients, the need for bilateral neck explorations has been questioned, and minimally invasive procedures based on unilateral approach have been introduced. These less invasive operations offer similar cure rates but result in quicker recovery time, shorted hospital stays, fewer complications, and have proved to be more cost-effective (4,5).
These minimally invasive parathyroidectomies typically require preoperative imaging studies for the localization of enlarged parathyroid glands and operative planning (6,7). Cervical ultrasonography (USG) when performed by an experienced sonographer is the least costly modality providing anatomical information, and together with [99mTc]sestamibi [multiplexed ion beam imaging (MIBI)] parathyroid scintigraphy, they are the main tests to locate the hyperfunctional glands (6). In a systematic literature review of 20,225 cases of pHPT, USG and MIBI showed a sensitivity of 78.5% and 88.4% for the detection of solitary adenomas but decreased to 34.9% and 44.5% for multiple gland hyperplasia disease, respectively (8). In a study of ectopic parathyroid glands, preoperative MIBI scans showed a higher sensitivity (89%) than USG (59%), but accuracy of detection varied according to location of ectopic tissue (thymus, mediastinum or retroesophageal space for MIBI and intrathyroidal glands for USG) (9). Combined MIBI scan and USG demonstrated a high positive predictive value (9).
In response to the search for more sensitive and accurate imaging techniques that guarantee the correct diagnosis even in the presence of small parathyroid lesions, in cases of ectopic glands, or after an unsuccessful neck examination, [18F]fluorocholine (FCH) positron emission tomography/computed tomography (PET/CT) has been recently investigated with encouraging results (10-12).
Radiolabelled choline PET/CT has been widely used to identify prostate cancer metastases. Nevertheless, it has also been useful in the identification of diseases such as parathyroid adenoma (13,14).
The uptake of radiolabelled choline is increased by upregulation of choline kinase and is related to PTH secretion in parathyroid hyperfunctioning glands, so radiolabelled choline PET works in the identification of this pathology (14,15). Numerous studies have demonstrated the high sensitivity of FCH PET/CT in patients with pHPT with negative, discordant first-line examinations or small adenomas (14,16).
The diagnostic accuracy of the three techniques (USG, MIBI, FCH PET/CT) in patients with pHPT has been compared in a few studies, in which FCH PET/CT has been found to be more accurate than the others, principally for ectopic or small parathyroid adenomas (17-19). To add evidence to the usefulness of these preoperative imaging techniques, the current prospective study was conducted to compare the diagnostic performance of USG, MIBI and FCH PET/CT in patients with pHPT undergoing parathyroid surgery. We present the following article in accordance with the STARD reporting checklist (available at https://gs.amegroups.com/article/view/10.21037/gs-22-198/rc).
Methods
Design
This study was prospectively carried out from January 2019 to September 2020 at the Departments of Nuclear Medicine, Endocrinology, and General Surgery of Hospital Clínic of Barcelona, in Barcelona, Spain. This study was conducted according to the guidelines of the Declaration of Helsinki (as revised in 2013). This study was approved by the Ethics Committee for Clinical Research of Hospital Clinic of Barcelona (protocol number V3-04/03/2022) and participants signed the written consent form. Diagnosis of pHPT was based on hypercalcemia or elevated serum PTH levels, enlarged parathyroid glands documented at surgery and histopathological confirmation. The lowering of serum PTH by 50% or more a subsequent postoperative stabilization of serum calcium (Ca) levels were considered to be signs of pHPT cure (17).
Patients
All patients who were clinically and biochemically diagnosed with pHPT (PTH >80 pg/mL and/or Ca >10.5 mg/mL without hypocalcaemic treatment) during this period, and who had been subjected to the three modalities of preoperative imaging (USG, MIBI, and FCH PET/CT) followed by parathyroid surgery, were included in the study (37 patients). Secondary or tertiary hyperparathyroidism, chronic kidney disease, and the presence of any other cancer, including thyroid and parathyroid carcinoma, were taken into consideration as exclusion factors. Data on previous thyroid/parathyroid surgery, serum PTH, Ca, and P levels, urine Ca excretion per 24 hours, bone mineral density (BMD) of the proximal femur and lumbar vertebrae, and urinary USG for skeletal and renal involvement were all gathered from all patients. Results of histopathological examination and clinical follow-up were also recorded.
Preoperative localization techniques
- Cervical USG was accomplished at the Department of Radiology of our institution by an experienced radiologist. The patient was in a supine position and the neck was hyperextended. A high-resolution linear probe with a frequency of 7–12 MHz (iU22, Phillips, Andover, MA, USA) was used. The examination field extended from the angles of the mandible to the sternum notch. For each of the potential locations, the radiologist scored whether hyperplastic parathyroid gland(s) were present (on the right and left sides of the thyroid bed and cervical ectopic glands). Homogenously hypoechoic lesions close to or in relation to the thyroid gland were used to detect enlarged parathyroid glands.
- Planar MIBI imaging with or without single photon emission computed tomography/computed tomography (SPECT/CT). Planar and pinhole images of the neck and thorax were captured over 5-min duration in 256×256 matrix using a one-headed gamma camera (E-Cam, Siemens, Erlangen, Germany) equipped with low energy and high-resolution collimator. Images were obtained at 15 min and 2 hours after injection of 24 mCi (888 MBq). Then, SPECT images were captured in a gamma camera (Symbia Intevo Bold, Siemens Healthineers, Erlangen, Germany) (120 projections in a non-circular orbit in 360°, 30 s/projection, in a 128×128 matrix with 3.30×3.30 mm2 pixel size), using a CT image (512×512 matrix size, 130 kV and CARE Dose4D) for attenuation correction and subsequent merging of the reconstructed image. Any abnormal tracer uptake focus with delayed image retention in the thyroid bed region or any possible site for ectopic adenoma was considered as positive finding for parathyroid adenoma. Image interpretation was performed by specialists in nuclear medicine [Nuria Sanchez (NS), Sebastian Casanueva (SC), Andres Perissinotti (AP), Sergi Vidal Sicart (SVS)]. Clinical information and additional imaging findings were accessible to the interpreters.
- FCH PET/CT was obtained with patients in 4-hour fasting conditions, at 60 min after intravenous administration of 370 MBq of FCH using hybrid PET/CT equipment (Biograph mCT TrueV, Siemens Medical Solutions USA, Inc.). Images obtained from the cranial vault to mid-thigh were revised in three planes (transaxial, coronal, and sagittal) by specialists in nuclear medicine (NS, SC, AP, SVS). Positive results were characterized as a localized uptake in the neck or mediastinum that was greater than the adjacent background activity and that coincided with a nodular lesion on the CT scan. To determine the maximum standardized uptake value (SUVmax), a three-dimensional spherical volume of interest was plotted over the entire lesion using FCH uptake. Clinical information and the reference standard results were presented to the test interpreters.
Surgery and histopathological findings
The same surgeon used USG, MIBI scintigraphy, and FCH PET/CT results from on-site open reading to plan and perform the surgical procedures. A retrothyroid minimally invasive method was used. Under general anesthesia, a transverse neck incision about 3–4 cm in length was made to perform the assessment for abnormal parathyroid glands.
To evaluate the effectiveness of preoperative imaging studies, four histopathological parameters were taken into account: (I) recognition of parathyroid tissue on frozen sections, (II) specific histopathological examination, (III) weight of excised parathyroid glands, and (IV) size of excised parathyroid glands. In cases of hemithyroidectomy or total thyroidectomy, a histological investigation of the removed thyroid tissue was carried out.
Statistical analysis
Frequencies and percentages are used to convey categorical data, and the mean and standard deviation (SD) or median and interquartile range (IQR) (25th–75th percentile) are used to express continuous data. The chi-square test was used for the comparison of categorical data and the paired t-test or the Wilcoxon signed-rank test for the comparison of continuous data according to conditions of application. The relationship between biochemical parameters and histological findings was evaluated with Pearson’s product-moment correlation coefficient (r). Indeterminate results were interpreted as false-positive or false-negative and included into the final analysis. Regarding the primary test being investigated, there were no missing data. Each imaging method’s sensitivity, specificity, positive and negative predictive values, and diagnostic accuracy were calculated. Tests with P<0.05 were considered statistically significant. Statistical analyses were done using SPSS version 24.0 (IMB Corp., Armonk, NY, USA).
Results
Clinical characteristics and histopathological findings
The study population included 37 patients (30 women, 7 men) with a mean age (±SD) of 62.9 (±9.1) years (range, 41.0–83.0 years). In all these patients, histological findings including final diagnosis and size and weight of each parathyroid gland were available. Table 1 shows the clinical characteristics of patients, biochemical parameters, and histological findings. The final diagnosis included parathyroid adenoma in 31 cases and hyperplasia in the remaining 6. There were 3 cases of ectopic parathyroid adenomas and 3 cases of multiglandular disease.
Table 1
| Variable | Value |
|---|---|
| Gender, n (%) | |
| Men | 7 (18.9) |
| Women | 30 (81.1) |
| Age (years), mean ± SD (range) | 62.9±9.1 (41.0–83.0) |
| Serum PTH levels (pg/mL), median (IQR) | |
| Preoperative | 151.0 (122.5–200.5) |
| Postoperative | 66.0 (47.5–95.0) |
| Serum calcium levels (mg/dL), mean ± SD (range) | |
| Preoperative | 10.7±0.7 (8.8–12.5) |
| Postoperative | 8.9±0.6 (7.1–10.4) |
| Parathyroid adenoma | |
| Size (cm), mean ± SD (range) | 1.8±0.8 (0.4–3.5) |
| Weight (g), median (IQR) | 0.8 (0.4–1.5) |
SD, standard deviation; PTH, parathyroid hormone; IQR, interquartile range.
Serum PTH levels decreased significantly after surgery, from a median (IQR) of 151.0 pg/mL (IQR, 122.5–200.5 pg/mL) preoperatively to 66.0 pg/mL (IQR, 47.5–95.0 pg/mL) postoperatively, with a median decrease of 105.0 pg/mL (IQR, 66.5–121.5 pg/mL) (P<0.001). Serum Ca levels also decreased significantly, from a mean (±SD) of 10.7 (±0.7) mg/dL to 8.9 (±0.6) mg/dL, with a mean (±SD) reduction of 1.7 (±0.8) mg/dL (P<0.001). The decrease of serum PTH level showed a positive correlation with parathyroid gland size (r=0.489; P=0.004) and weight (r=0.465; P=0.015). The preoperative Ca level was also correlated with gland size (r=0.421; P=0.009). The mean (±SD) SUVmax value was 9.1 (±4.0) (range, 3.2–20.0) and also correlated significantly with gland size (r=0.375; P=0.027) and gland weight (r=0.397; P=0.036).
On the other hand, the size of the parathyroid glands was significantly greater in patients with adenoma than in those with hyperplasia [1.97 (0.72) vs. 1.02 (0.56) cm; P=0.004].
Diagnostic performance of the three imaging modalities
No adverse events were reported from any of the preoperative imaging tests. Preoperatively, USG, MIBI and FCH PET/CT were able to locate pathological parathyroid glands in 27.0% (10/37), 59.5% (22/37), and 81.1% (30/37) of cases, respectively. The results of the three imaging modalities were analyzed per patient (35 out of the 37 in whom a positive parathyroid adenoma was found) and per-lesion (38 lesions correlated with a positive parathyroid adenoma) basis. The sensitivity was 32.4% for USG, 57.9% for MIBI, and 92.1% for FCH PET/CT, with an overall diagnostic accuracy of 79.0%, 85.7%, and 96.4% for USG, MIBI, and FCH PET/CT, respectively. False negative in parathyroid MIBI scintigraphy are caused by the existence of a cyst in the proliferative parathyroid lesions, as well as their small size and multiplicity. False positives could have been due to localization in a thyroid nodule or lymph node (Table 2).
Table 2
| Technique | TP | TN | FP | FN | Sensitivity | Specificity | PPV | NPV | Accuracy |
|---|---|---|---|---|---|---|---|---|---|
| USG | 11 | 87% | 3 | 23 | 32.4% | 96.7% | 78.6% | 79.1% | 79.0% |
| MIBI | 22 | 98% | 4 | 16 | 57.9% | 96.1% | 84.6% | 86.0% | 85.7% |
| FCH PET/CT | 35 | 100% | 2 | 3 | 92.1% | 98.0% | 94.6% | 97.1% | 96.4% |
TP, FP and FN are expressed in absolute numbers. USG, ultrasonography; MIBI, multiplexed ion beam imaging; FCH PET/CT, [18F]fluorocholine positron emission tomography/computed tomography; TP, true positive; TN, true negative; FP, false positive; FN, false negative; PPV, positive predictive value; NPV, negative predictive value.
Intraoperative findings confirmed 3 ectopic parathyroid adenomas which were correctly located by USG, MIBI and FCH PET/CT in 1 (33.3%), 2 (66.7%) and 3 (100%) of the patients, respectively. Neither USG nor MIBI were able to locate both pathological parathyroid glands in those patients with multiglandular disease, while FCH PET/CT correctly located one patient (1/3, 33.3%). In the 6 patients with hyperplasia, USG and MIBI did not find any pathological glands (0%, 0/6), whereas, in 50% of patients, FCH PET/CT was able to determine the proper diagnosis (3/6).
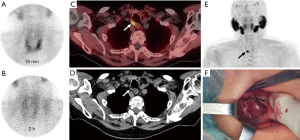
Finally, the mean size of the parathyroid gland was significantly greater in those patients in whom FCH PET/CT correctly localized the gland [1.95 (0.76) cm] than in those in which FCH PET/CT failed to localize the gland [1.26 (0.72) cm] (P=0.036). In addition, the presence of concomitant pathology of the thyroid gland (multinodular goiter) decreased the sensitivity of FCH PET/CT from 92.1% to 54% (P=0.007). The images of an illustrative case of a 62-year-old woman with biochemical evidence of pHPT are shown in Figure 1.
Discussion
In this series of patients with pHPT, FCH PET/CT was superior to MIBI scintigraphy and neck USG for the preoperative identification of parathyroid lesions, particularly in cases of ectopic glands, multiglandular disease and parathyroid hyperplasia. Successful preoperative localization of abnormal glands probably contributes to reducing the morbidity of surgery, allowing the surgeon to perform a more selective and safe procedure (20). The focused surgical approach or targeted parathyroidectomy eliminates bilateral exploration or unnecessary dissection of multiple glands. However, the accuracy and reliability of preoperative localization tests have been essential for further advances in minimally invasive parathyroid surgery (21). In fact, minimally invasive parathyroidectomy is the procedure of choice in many centers based on the assumption that the parathyroid gland or glands have been identified preoperatively (1). The exact modality for preoperative identification of abnormal parathyroid tissue depends on technological availability, with high-resolution USG and MIBI scintigraphy used in most major clinical centers.
The present findings of a higher diagnostic performance of FCH PET/CT as compared with USG and MIBI are in agreement with other studies. The superior ability of radiolabelled choline PET to identify hyperfunctioning parathyroid glands in pHPT was shown in a meta-analysis of 14 studies with 517 patients, in which 95% sensitivity, 97% positive predictive value, and 91% detection rate was reported (15). These data confirmed the findings of a previous meta-analysis of 8 studies with 272 patients (22). FCH PET/CT also delivers high rates of sensitivity, specificity, positive predictive value, and diagnostic accuracy in patients with discrepant results on scintigraphy or USG, hyperplasia or multiple lesions, persistent or recurrent HPT, small or ectopic adenomas, and normocalcemic HPT (23-27).
Some studies have compared FCH PET/CT accuracy with other imaging techniques in patients with hyperparathyroidism. In 17 patients with pHPT in 11, lithium-associated hyperparathyroidism in 1, and secondary hyperparathyroidism in 5, the patient-based sensitivity was 88% for open reading FCH PET/CT, 69% for MIBI, and 38% for USG, although correlation between FCH uptake and PTH serum level was not found to be statistically significant (19). In a prospective study of 54 patients with pHPT, the diagnostic accuracy in the patient-wise analysis was 62.9% for USG, 79.6% for MIBI, and 96.5% for FCH PET/CT (17), which are quite similar to the percentages of 79%, 85.7%, and 96.4% found in our study. In patients with ectopic lesions, FCH PET/CT also showed 100% sensitivity (17), in line with the findings of the current study. Moreover, in a clinical series of 35 pHPT patients with inconclusive USG who experienced MIBI SPECT and FCH PET/CT, the sensitivity, positive predictive value, and diagnostic accuracy were higher in FCH PET/CT; in this study, SUVmax of the parathyroids correlated with illness severity in relation to serum PTH levels and lumbar and femoral BMD scores (28). In 82 patients with pHPT in which FCH PET/CT and [99mTc]-MIBI/tetrofosmin SPECT/CT was compared, FCH PET/CT showed a better performance in the location of parathyroid lesions, with higher sensitivity, positive predictive value, and diagnostic accuracy (18).
The relatively small study population and the single-center design are the main limitations of this study. However, in contrast to other reports (17), the role of FCH PET/CT could be assessed in patients with multiglandular disease and hyperplasia, and in both conditions, FCH PET/CT performed diagnostically more effectively than USG and MIBI.
Conclusions
In this study, FCH PET/CT demonstrated superior diagnostic performance over cervical USG and MIBI scintigraphy in the preoperative localization of parathyroid lesions in patients with pHPT undergoing parathyroid surgery. The superiority of FCH PET/CT seems particularly useful in multiglandular disease and parathyroid hyperplasia. These results may support the position of FCH PET/CT as the best choice for evaluating parathyroid disease prior to surgery in pHPT patients scheduled for curative parathyroidectomy.
Acknowledgments
The authors thank Marta Pulido, MD, for editorial assistance.
Funding: None.
Footnote
Reporting Checklist: The authors have completed the STARD checklist. Available at https://gs.amegroups.com/article/view/10.21037/gs-22-198/rc
Data Sharing Statement: Available at https://gs.amegroups.com/article/view/10.21037/gs-22-198/dss
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://gs.amegroups.com/article/view/10.21037/gs-22-198/coif). The authors have no conflicts of interest to declare.
Ethical Statement:
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Bilezikian JP, Bandeira L, Khan A, et al. Hyperparathyroidism. Lancet 2018;391:168-78. [Crossref] [PubMed]
- Rodrigo JP, Hernandez-Prera JC, Randolph GW, et al. Parathyroid cancer: An update. Cancer Treat Rev 2020;86:102012. [Crossref] [PubMed]
- Chen H. Surgery for primary hyperparathyroidism: what is the best approach? Ann Surg 2002;236:552-3. [Crossref] [PubMed]
- Goldstein RE, Blevins L, Delbeke D, et al. Effect of minimally invasive radioguided parathyroidectomy on efficacy, length of stay, and costs in the management of primary hyperparathyroidism. Ann Surg 2000;231:732-42. [Crossref] [PubMed]
- Laird AM, Libutti SK. Minimally Invasive Parathyroidectomy Versus Bilateral Neck Exploration for Primary Hyperparathyroidism. Surg Oncol Clin N Am 2016;25:103-18. [Crossref] [PubMed]
- Wilhelm SM, Wang TS, Ruan DT, et al. The American Association of Endocrine Surgeons Guidelines for Definitive Management of Primary Hyperparathyroidism. JAMA Surg 2016;151:959-68. [Crossref] [PubMed]
- Cheung K, Wang TS, Farrokhyar F, et al. A meta-analysis of preoperative localization techniques for patients with primary hyperparathyroidism. Ann Surg Oncol 2012;19:577-83. [Crossref] [PubMed]
- Ruda JM, Hollenbeak CS, Stack BC Jr. A systematic review of the diagnosis and treatment of primary hyperparathyroidism from 1995 to 2003. Otolaryngol Head Neck Surg 2005;132:359-72. [Crossref] [PubMed]
- Roy M, Mazeh H, Chen H, et al. Incidence and localization of ectopic parathyroid adenomas in previously unexplored patients. World J Surg 2013;37:102-6. [Crossref] [PubMed]
- Vellani C, Hodolič M, Chytiris S, et al. Early and Delayed 18F-FCH PET/CT Imaging in Parathyroid Adenomas. Clin Nucl Med 2017;42:143-4. [Crossref] [PubMed]
- Huber GF, Hüllner M, Schmid C, et al. Benefit of 18F-fluorocholine PET imaging in parathyroid surgery. Eur Radiol 2018;28:2700-7. [Crossref] [PubMed]
- Christakis I, Khan S, Sadler GP, et al. 18Fluorocholine PET/CT scanning with arterial phase-enhanced CT is useful for persistent/recurrent primary hyperparathyroidism: first UK case series results. Ann R Coll Surg Engl 2019;101:501-7. [Crossref] [PubMed]
- Mapelli P, Busnardo E, Magnani P, et al. Incidental finding of parathyroid adenoma with 11C-choline PET/CT. Clin Nucl Med 2012;37:593-5. [Crossref] [PubMed]
- Giovanella L, Bacigalupo L, Treglia G, et al. Will 18F-fluorocholine PET/CT replace other methods of preoperative parathyroid imaging? Endocrine 2021;71:285-97. [Crossref] [PubMed]
- Treglia G, Piccardo A, Imperiale A, et al. Diagnostic performance of choline PET for detection of hyperfunctioning parathyroid glands in hyperparathyroidism: a systematic review and meta-analysis. Eur J Nucl Med Mol Imaging 2019;46:751-65. [Crossref] [PubMed]
- Ballester Vázquez E, Pérez García JI, López Mora DA, et al. Identification of Occult Adenomas in Primary Hyperparathyroidism With 18F-fluorocholine PET/CT. Cirugía Española 2020;98:395-402. [Crossref] [PubMed]
- Thanseer N, Bhadada SK, Sood A, et al. Comparative Effectiveness of Ultrasonography, 99mTc-Sestamibi, and 18F-Fluorocholine PET/CT in Detecting Parathyroid Adenomas in Patients With Primary Hyperparathyroidism. Clin Nucl Med 2017;42:e491-7. [Crossref] [PubMed]
- Beheshti M, Hehenwarter L, Paymani Z, et al. 18F-Fluorocholine PET/CT in the assessment of primary hyperparathyroidism compared with 99mTc-MIBI or 99mTc-tetrofosmin SPECT/CT: a prospective dual-centre study in 100 patients. Eur J Nucl Med Mol Imaging 2018;45:1762-71. [Crossref] [PubMed]
- Michaud L, Balogova S, Burgess A, et al. A Pilot Comparison of 18F-fluorocholine PET/CT, Ultrasonography and 123I/99mTc-sestaMIBI Dual-Phase Dual-Isotope Scintigraphy in the Preoperative Localization of Hyperfunctioning Parathyroid Glands in Primary or Secondary Hyperparathyroidism. Medicine (Baltimore) 2015;94:e1701. [Crossref] [PubMed]
- Mariani G, Gulec SA, Rubello D, et al. Preoperative localization and radioguided parathyroid surgery. J Nucl Med 2003;44:1443-58. [PubMed]
- Noureldine SI, Gooi Z, Tufano RP. Minimally invasive parathyroid surgery. Gland Surg 2015;4:410-9. [PubMed]
- Kim SJ, Lee SW, Jeong SY, et al. Diagnostic Performance of F-18 Fluorocholine PET/CT for Parathyroid Localization in Hyperparathyroidism: a Systematic Review and Meta-Analysis. Horm Cancer 2018;9:440-7. [Crossref] [PubMed]
- Boccalatte LA, Higuera F, Gómez NL, et al. Usefulness of 18F-Fluorocholine Positron Emission Tomography-Computed Tomography in Locating Lesions in Hyperparathyroidism: A Systematic Review. JAMA Otolaryngol Head Neck Surg 2019;145:743-50. [Crossref] [PubMed]
- Michaud L, Burgess A, Huchet V, et al. Is 18F-fluorocholine-positron emission tomography/computerized tomography a new imaging tool for detecting hyperfunctioning parathyroid glands in primary or secondary hyperparathyroidism? J Clin Endocrinol Metab 2014;99:4531-6. [Crossref] [PubMed]
- Kluijfhout WP, Vorselaars WM, van den Berk SA, et al. Fluorine-18 fluorocholine PET-CT localizes hyperparathyroidism in patients with inconclusive conventional imaging: a multicenter study from the Netherlands. Nucl Med Commun 2016;37:1246-52. [Crossref] [PubMed]
- Bossert I, Chytiris S, Hodolic M, et al. PETC/CT with 18F-Choline localizes hyperfunctioning parathyroid adenomas equally well in normocalcemic hyperparathyroidism as in overt hyperparathyroidism. J Endocrinol Invest 2019;42:419-26. [Crossref] [PubMed]
- Grimaldi S, Young J, Kamenicky P, et al. Challenging pre-surgical localization of hyperfunctioning parathyroid glands in primary hyperparathyroidism: the added value of 18F-Fluorocholine PET/CT. Eur J Nucl Med Mol Imaging 2018;45:1772-80. [Crossref] [PubMed]
- Araz M, Soydal Ç, Özkan E, et al. The efficacy of fluorine-18-choline PET/CT in comparison with 99mTc-MIBI SPECT/CT in the localization of a hyperfunctioning parathyroid gland in primary hyperparathyroidism. Nucl Med Commun 2018;39:989-94. [Crossref] [PubMed]


