
Analysis of the accuracy of ultrasound elastography and BI-RADS classification of breast masses located within the superficial fat layer of the glands
Introduction
Although breast cancer is the most common malignancy in women (1), its 5-year survival rate exceeds 90% if detected early (2). Therefore, early detection of breast cancer is important for prognosis. Ultrasound and mammography were the most commonly used methods of breast cancer examination. Because the breasts of most Chinese women are relatively small and dense, mammography was easy to miss breast tumors (3). Because of its convenience, no radiation effects, low cost, and rapidity, ultrasonography has become the preferred method for screening breast cancer in China (4,5).
Given the widespread use of breast ultrasound, the Breast Imaging Reporting and Data System (BI-RADS) has been widely used and standardized to guide the management of breast disease (6,7). Numerous studies have reported that breast ultrasound BI-RADS classification is effective for the differential diagnosis of benign and malignant breast masses (7-9). However, only about 15% of breast tumors in BI-RADS category 4 are malignant, while the majority of benign breast tumors suffer from unnecessary biopsy or surgery, which requires more accurate diagnostic methods (10). Ultrasound elastography can be used to assess the stiffness of breast masses, and many studies have reported that it can improve the accuracy of ultrasound in distinguishing benign from malignant breast tumors (10-15). Studies have shown that ultrasound elastography can be used to upgrade or downgrade the ultrasound BI-RADS classification of breast tumors (16-19). Ultrasound elastography features of breast masses have been incorporated into the latest version of BI-RADS (20). The surrounding tissue of lesions located in the mammary fat layer is mainly fat, not mammary glands. The growth environment of breast masses located in the fat layer are different from that in the breast glands. Since fat is usually softer than the breast glands, the mass growth pattern may be different, which may affect the evaluation of BI-RADS classification and ultrasound elasticity. Are the currently used BI-RADS classifications and ultrasound elasticity appropriate for such lesions? The BI-RADS classification and ultrasound elasticity assessment of breast masses within the fat layer have not been reported in the literature. In the present study, we discuss the value of elastography and BI-RADS classification in the evaluation of masses in the superficial fat layer of the breast. We present the following article in accordance with the STARD reporting checklist (available at https://gs.amegroups.com/article/view/10.21037/gs-22-503/rc).
Methods
Patients
The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the ethics committee of The Ningbo First Hospital (No. 2022RS049). Individual consent for this retrospective analysis was waived.
A cross-sectional double-blind study was used. From January 2014 to January 2022 in our hospital, all patients with breast masses located in the superficial fat layer of the glands were pathologically confirmed as the research subjects. Using histopathology as the gold standard, we retrospectively analyzed whether the ultrasound elastography and BI-RADS classification results were consistent with the pathological results.
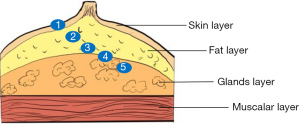
The selection criteria were as follows: (I) all patients underwent routine ultrasound and ultrasound elastography examinations, and pathological results were obtained (Mammotome breast biopsy or surgical resection); and (II) breast masses need to be located within the fat layer on the surface of the gland (Figure 1). The exclusion criteria were as follows: (I) breast masses with no pathological findings; and (II) breast masses located in the glandular or skin layer of the breast (Figure 1). Seventy-five breast masses within the fat layer that met inclusion criteria were included in the study. The average age of the patients was 46.7 years (range, 19–78 years). The average maximum diameter of the 75 breast masses was 13.4 mm (range, 4–45 mm).
Ultrasound examinations
All patients in the study underwent routine ultrasound and ultrasound elastography. When a breast mass was detected, the position, size, edge, echo, aspect ratio, calcification, and blood flow of the mass were recorded. Ultrasound examinations were performed using a 7–13 MHz linear transducer (EUB 8500; Hitachi Medical Systems GmbH, Tokyo, Japan). Compression criteria for ultrasound elastography procedures: hold the probe to compress the lesion according to the standard (the indicator bar displaying 3 or 4). The sampling frame needs to enclose the mass and its surrounding tissues, and the ultrasound elastography image and the gray-scale ultrasound image are displayed on the machine screen at the same time. Ultrasound elastography images are shown from red to blue; red represents the softest mass and blue represents the hardest mass.
According to the 5-point scoring scale proposed by Itoh et al. (21). Score 1: the entire mass is evenly shaded in green, as the surrounding normal breast tissue (even strain within the entire mass); score 2: the mass is a mosaic pattern of green and blue (strain throughout the mass with some strain-free areas); score 3: the central part of the mass is blue, and the peripheral part is green (strain only in the periphery of the mass but not in the center); score 4: the entire mass is blue (no strain within the entire mass); and score 5: the entire mass and its surroundings are blue (no strain within the entire mass and adjacent surrounding tissue). Ultrasound elasticity score ≤3 was considered benign, and ≥4 was considered malignant.
On the conventional ultrasound scans, lesions were characterized using BI-RADS criteria. The lesions were classified as category 2–5 lesions according to the 5th edition of the BI-RADS criteria. Category 2 is benign (follow up is recommended), category 3 is probably benign (short-term follow-up is recommended), category 4 is suspicion of malignancy (needs biopsy) and category 5 is highly suggestive of malignancy (needs biopsy). Category 4 is further divided into 4a (probability of malignancy: 3–10%), 4b (probability of malignancy: 11–50%), and class 4c highly suspicious of malignancy (probability of malignancy: 51–94%).
The BI-RADS classification was evaluated by 2 sonographers with 10 years of experience in breast ultrasonography, and reach an agreement. None of the 2 sonographers knew the pathological diagnosis of the breast masses. Ultrasound elastography was evaluated by another physician with 5 years of experience in ultrasound elastography, who was also blind.
Statistical analysis
All data were analyzed using SPSS version 13.0 statistical software (Chicago, IL, USA). Statistical analysis was performed, and histopathology results were considered the diagnostic gold standard. The numerical data were expressed as the mean ± SD. A P value of less than 0.05 was considered statistically significant.
Results
The histopathology of 75 breast masses showed that 73 were benign and 2 were malignant. There was 1 case of invasive ductal carcinoma, 1 of solid papillary carcinoma, 53 of fibroadenoma, 9 of breast cyst, 7 of fibroadenosis, 3 of intraductal papilloma, and 1 of breast inflammatory lesions.
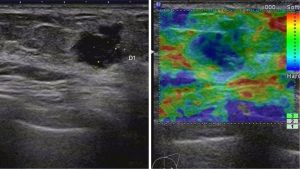
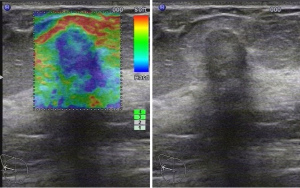
We analyzed and summarized the ultrasound imaging characteristics of the 75 breast masses (Table 1). One case of invasive ductal carcinoma (maximum diameter: 12 mm, patient age: 72 years) showed on ultrasound that the margin of the mass was not smooth, the aspect ratio was greater than 1, the shape was irregular, no calcification, and little blood flow. The BI-RADS classification was 4c, and ultrasound elastography indicated a score of 4. This case of invasive ductal carcinoma showed typical malignant features on ultrasound and elastography (Figure 2). The ultrasound image of 1 case of solid papillary carcinoma (maximum diameter: 16 mm, patient age: 68 years) showed a clear boundary, irregular shape, aspect ratio <1, no calcification, and little blood flow. The BI-RADS classification was 4a, and ultrasound elastography indicated a score of 4. Of the 75 masses, 0% were classified as BI-RADS categories 2 or 5. In total, 40% (30/75) of masses were classified as BI-RADS 3 (malignant probability: 0%), 56% (42/75) were classified as BI-RADS 4a (malignant probability: 2.4%) (Figures 3,4), 2.7% (2/75) were classified as BI-RADS 4b (malignant probability: 0%), and 1.3% (1/75) were classified as BI-RADS 4c (malignant probability: 100%).
Table 1
| Characteristics | Subtypes | Numbers |
|---|---|---|
| Age (years), mean ± SD | 46.7±15.9 | |
| Location | Right | 32 |
| Left | 43 | |
| Maximum diameter of lesion (mm), mean ± SD | 13.4±6.5 | |
| Echoes | Hypoechoic | 75 |
| Other | 0 | |
| Margin | Well-defined | 74 |
| Ill-defined | 1 | |
| Shape | Regular | 50 |
| Irregular | 25 | |
| Aspect ratio | Taller than wide | 18 |
| Wider than tall | 57 | |
| Rear echo characteristics | Normal | 72 |
| Rear shadow | 3 | |
| Calcification | Microcalcification | 6 |
| Macrocalcification | 11 | |
| No | 58 | |
| Color Doppler flow imaging | No blood flow | 48 |
| Little blood flow | 17 | |
| Enriched blood flow | 10 | |
| Ultrasound elastography (score) | 1 | 4 |
| 2 | 27 | |
| 3 | 8 | |
| 4 | 36 | |
| 5 | 0 | |
| BI-RADS category | 2 | 0 |
| 3 | 30 | |
| 4a | 42 | |
| 4b | 2 | |
| 4c | 1 | |
BI-RADS, Breast Imaging Reporting and Data System.
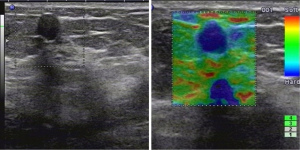
According to the BI-RADS classification and treatment principle, 60% (45/75) of the masses were classified into category 4 and require breast biopsy. But only 4.4% (2/45) of these masses were malignant, and 95.6% (43/45) were overtreated.
A total of 52.0% (39/75) cases of ultrasound elastography ≤3 points, histopathological findings were benign. A total of 48.0% (36/75) cases were scored as 4 points on ultrasound elastography. Pathological results showed that only 5.6% (2/36) of these masses were malignant, and 94.4% (34/36) of the masses were misdiagnosed as malignant by ultrasound elastography.
The BI-RADS classification was downgraded according to the ultrasound elasticity ≤3 points, and the BI-RADS classification was upgraded according to the ultrasound elasticity ≥4 points. According to ultrasound elastography-adjusted BI-RADS classifications 2, 3, 4a, 4b, 4c, and 5, the malignancy probability was 0% (0/18), 0% (0/22), 0% (0/12), 5% (1/20), 0% (0/2), and 100% (1/1), respectively. According to the BI-RADS classification and treatment principle, 46.7% (35/75) of the masses were classified into categories 4 or 5 and require breast biopsy. But only 5.7% (2/35) of these masses were malignant, and 94.3% (33/35) were overtreated.
The BI-RADS classification was downgraded according to ultrasound elasticity ≤3 points, and the BI-RADS classification was unchanged with ultrasound elasticity ≥4 points. According to ultrasound elastography-adjusted BI-RADS classifications 2, 3, 4a, 4b, and 4c, the malignancy probability was 0% (0/18), 0% (0/33), 4.8% (1/21), 0% (0/2), and 100% (1/1), respectively. According to the BI-RADS classification and treatment principle, 32.0% (24/75) of the masses were classified into category 4 and require breast biopsy. But only 8.3% (2/24) of these masses were malignant, and 91.7% (22/24) were overtreated.
With the exception of 1 case of invasive ductal carcinoma with an unclear boundary (BI-RADS 4c), the remaining 74 masses showed clear boundaries. Among them, 59.5% (44/74) were classified as BI-RADS 4 (only 1 case of solid papillary carcinoma; the others were benign). The main reasons for being classified as BI-RADS 4 were irregular morphology, aspect ratio >1, and microcalcification. If we consider masses with well-defined margins and within the fat layer on the surface of the breast glands as likely to be benign (BI-RADS 3), the probability of malignancy is 1.4%. If such breast masses are ill-defined margins, the BI-RADS classification criteria are used. According to this BI-RADS classification, only 1.3% (1/75) of patients required biopsy.
Discussion
Most of the breast lesions commonly seen are located in the glands, but some breast lesions are completely located in the fat layer. We speculate that the breast mass in the fat layer may originate from a small amount of glands extending into the fat layer, or due to aging the glands degenerate, and the mass does not degenerate with the glands and remains in the fat layer.
The BI-RADS classification is widely used worldwide (7-9). BI-RADS classification criteria are as follows (7,8): category 1: no clinical signs and no abnormal findings on ultrasonography; category 2: malignant probability of 0%; category 3: probability of malignancy <3%; category 4a: probability of malignancy of 3–10%; category 4b: probability of malignancy of 11–50%; category 4c: probability of malignancy of 51–94%; and category 5: malignant probability ≥95%. However, our study shows that such masses (located in the fat layer) BI-RADS classification 3, 4a, 4b, 4c, the probability of malignancy is 0% (0/30), 2.4% (1/42), 0% (0/2), and 100% (1/1), respectively.
Such masses have a low probability of malignancy and are significantly misclassification by BI-RADS. The probability of developing breast cancer increases with age (22). Although the majority of breast masses in this study were BI-RADS categories 3 and 4a, the prevalence of older age led to unnecessary surgical resection or Mammotome rotational biopsy in most patients.
The BI-RADS classification can be downgraded if elastography shows a soft mass, and the BI-RADS classification can be upgraded if elastography shows a hard mass (16-19). This study shows that ultrasound elastography can easily misdiagnose benign masses as malignant. Reasons for analysis: The breast masses selected in this study were located in the fat layer, and the surrounding tissue was fat rather than breast glands. The principle of ultrasound elastography to evaluate breast masses is that breast cancer tissue is stiffer than the surrounding normal glandular tissue. When compressed, softer tissue deforms to a greater degree and harder tissue deforms to a lesser extent (21). The hardness of the lesion depends on the difference between the softness and hardness of the surrounding tissue. The mass is obviously harder than the surrounding tissue, and the location of the mass appears blue on the screen (indicates a mass that is hard). Fat tissue is not only softer than breast cancer, but also softer than normal breast tissue and benign masses (23). Therefore, ultrasound elastography of benign and malignant breast masses located in the fat layer showed that the masses were hard.
If we upgrade the BI-RADS classification based on ultrasound elastography ≥4 points, this would allow more benign tumors to be classified as class 4 (A total of 34 category 4 masses; the probability of malignancy is only 2.9%), which would lead to unnecessary surgery or biopsy. The BI-RADS classification was downgraded by ultrasound elastography ≤3 points, but not upgraded. This reduces the number of needle biopsies of breast lumps. However, 32% (24/75) of patients were still classified as category 4 (malignant probability was only 8.3%). Still 91.7% (22/24) were overtreated. Neither the ultrasound elastography nor the BI-RADS classification were wrong in assessing breast masses within the fat layer.
In the present study, of the 75 masses, only 1 had unclear margins; the others all showed clear margins. The pathology of the mass with unclear margins was invasive ductal carcinoma, and ultrasound showed typical malignant features (BI-RADS 4c). Only 1 of the remaining 74 masses was malignant. Among them, only 1 malignant mass was a solid papillary carcinoma with a low degree of malignancy. If we consider the masses with well-defined margins and within the fat layer on the surface of the breast glands as likely to be benign (BI-RADS category 3), the probability of malignancy is 1.4%. This is consistent with the BI-RADS classification probability of malignancy. This minimizes the biopsy rate for such masses. For breast masses within the fat layer, a short-term follow-up observation may be reasonable.
The present study had several limitations. First, the sample of malignant cases was limited, and large samples are needed for further research and confirmation. Second, this study was a retrospective study and requires further confirmation by a large-scale, multicenter prospective study. Third, because ultrasound is the first choice for breast examination in China, mammography and magnetic resonance data for the study are lacking.
Conclusions
The findings of this study suggest that breast masses located in the fat layer are prone to be classified into category 4 by BI-RADS and thus be subjected to unnecessary biopsies. Ultrasound elastography can easily misdiagnose benign masses as malignant. It is suggested that ultrasound elastography can downgrade the BI-RADS classification, but not upgrade it. It is more reasonable for these breast masses to be classified into BI-RADS category 3 for follow-up observation when the boundary is clear, therefore avoiding unnecessary biopsy or surgery.
Acknowledgments
The authors thank Dr. Feng Mao and Dr. Jian Lu from Ningbo First Hospital for their analysis of the images.
Funding: The research was supported by the Ningbo Science and Technology Bureau Fund (grant Nos. 2019C50037 and 2019A610308).
Footnote
Reporting Checklist: The authors have completed the STARD reporting checklist. Available at https://gs.amegroups.com/article/view/10.21037/gs-22-503/rc
Data Sharing Statement: Available at https://gs.amegroups.com/article/view/10.21037/gs-22-503/dss
Conflicts of Interest: Both authors have completed the ICMJE uniform disclosure form (available at https://gs.amegroups.com/article/view/10.21037/gs-22-503/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the ethics committee of The Ningbo First Hospital (No. 2022RS049). Individual consent for this retrospective analysis was waived.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Jemal A, Murray T, Ward E, et al. Cancer statistics, 2005. CA Cancer J Clin 2005;55:10-30. [Crossref] [PubMed]
- Brenner H, Gondos A, Arndt V. Recent major progress in long-term cancer patient survival disclosed by modeled period analysis. J Clin Oncol 2007;25:3274-80. [Crossref] [PubMed]
- Saarenmaa I, Salminen T, Geiger U, et al. The effect of age and density of the breast on the sensitivity of breast cancer diagnostic by mammography and ultasonography. Breast Cancer Res Treat 2001;67:117-23. [Crossref] [PubMed]
- Parajuly SS, Lan PY, Yan L, et al. Breast elastography: a hospital-based preliminary study in China. Asian Pac J Cancer Prev 2010;11:809-14. [PubMed]
- Jiang T, Jiang Y, Chen W, et al. Chinese association of ultrasound in medicine and engineering, superficial organs and peripheral vessels committee expert consensus on clinical frequently asked questions in breast ultrasonography, June 2018. J Cancer Res Ther 2018;14:1463-8. [Crossref] [PubMed]
- Lee SE, Moon JE, Rho YH, et al. Which supplementary imaging modality should be used for breast ultrasonography? Comparison of the diagnostic performance of elastography and computer-aided diagnosis. Ultrasonography 2017;36:153-9. [Crossref] [PubMed]
- Mercado CL. BI-RADS update. Radiol Clin North Am 2014;52:481-7. [Crossref] [PubMed]
- Wen W, Liu J, Wang J, et al. A National Chinese Survey on Ultrasound Feature Interpretation and Risk Assessment of Breast Masses Under ACR BI-RADS. Cancer Manag Res 2021;13:9107-15. [Crossref] [PubMed]
- Merchant K, Omar L, Hayes J, et al. ACR BI-RADS Category 3 Lesions in Women Younger Than 30: Follow-up Outcomes and Factors Associated With Biopsy. J Ultrasound Med 2021;40:2699-707. [Crossref] [PubMed]
- Liu XJ, Zhu Y, Liu PF, et al. Elastography for breast cancer diagnosis: a useful tool for small and BI-RADS 4 lesions. Asian Pac J Cancer Prev 2014;15:10739-43. [Crossref] [PubMed]
- Zhao W, Yan K, Liu Y, et al. Contrast ultrasound versus ultrasound elastography for diagnosis of breast lumps: A cross-sectional study. Medicine (Baltimore) 2019;98:e16132. [Crossref] [PubMed]
- Georgieva M, Prantl L, Utpatel K, et al. Diagnostic performance of ultrasound strain elastography for differentiation of malignant breast lesions. Clin Hemorheol Microcirc 2019;71:237-47. [Crossref] [PubMed]
- Kokubu Y, Yamada K, Tanabe M, et al. Evaluating the usefulness of breast strain elastography for intraductal lesions. J Med Ultrason (2001) 2021;48:63-70. [Crossref] [PubMed]
- Kanagaraju V, Dhivya B, Devanand B, et al. Utility of Ultrasound Strain Elastography to Differentiate Benign from Malignant Lesions of the Breast. J Med Ultrasound 2021;29:89-93. [Crossref] [PubMed]
- Hong S, Li W, Gao W, et al. Diagnostic performance of elastography for breast non-mass lesions: A systematic review and meta-analysis. Eur J Radiol 2021;144:109991. [Crossref] [PubMed]
- Reghunath A, Mittal MK, Chintamani C, et al. Novel approach in the evaluation of ultrasound BI-RADS 3 & 4 breast masses with a combination method of elastography & Doppler. Indian J Med Res 2021;154:355-66. [PubMed]
- Chiorean AR, Szep MB, Feier DS, et al. Impact of Strain Elastography on BI-RADS classification in small invasive lobular carcinoma. Med Ultrason 2018;20:148-53. [Crossref] [PubMed]
- Li H, Cheng C, Wang Y, et al. Combined diagnosis of ultrasonic elastography and BI-RADS classification increases diagnostic value in female patients with breast neoplasms. Am J Transl Res 2021;13:11758-63. [PubMed]
- Wei Q, Yan YJ, Wu GG, et al. Added Value of a New Strain Elastography Technique in Conventional Ultrasound for the Diagnosis of Breast Masses: A Prospective Multicenter Study. Front Oncol 2021;11:779612. [Crossref] [PubMed]
- Barr RG, Nakashima K, Amy D, et al. WFUMB guidelines and recommendations for clinical use of ultrasound elastography: Part 2: breast. Ultrasound Med Biol 2015;41:1148-60. [Crossref] [PubMed]
- Itoh A, Ueno E, Tohno E, et al. Breast disease: clinical application of US elastography for diagnosis. Radiology 2006;239:341-50. [Crossref] [PubMed]
- Westphal T, Rinnerthaler G, Mlineritsch B. Adjuvant medical treatment for breast cancer in elderly and old women. Memo 2016;9:17-9. [Crossref] [PubMed]
- Krouskop TA, Wheeler TM, Kallel F, et al. Elastic moduli of breast and prostate tissues under compression. Ultrason Imaging 1998;20:260-74. [Crossref] [PubMed]
(English Language Editor: R. Scott)


